- Research
- Open access
- Published:
Driving the determinants of older people’s mental health in the context of urban resilience: a scoping review
BMC Geriatrics volume 23, Article number: 711 (2023)
Abstract
Background
Population aging is a pervasive phenomenon occurring rapidly worldwide, while sustainable development goals are considered the mental health among older adults.
Methods
To investigate the factors affecting mental health, we conducted a scoping review of the 47 papers published between 2015 and 2022 to explore various dimensions affecting older adults’ mental health.
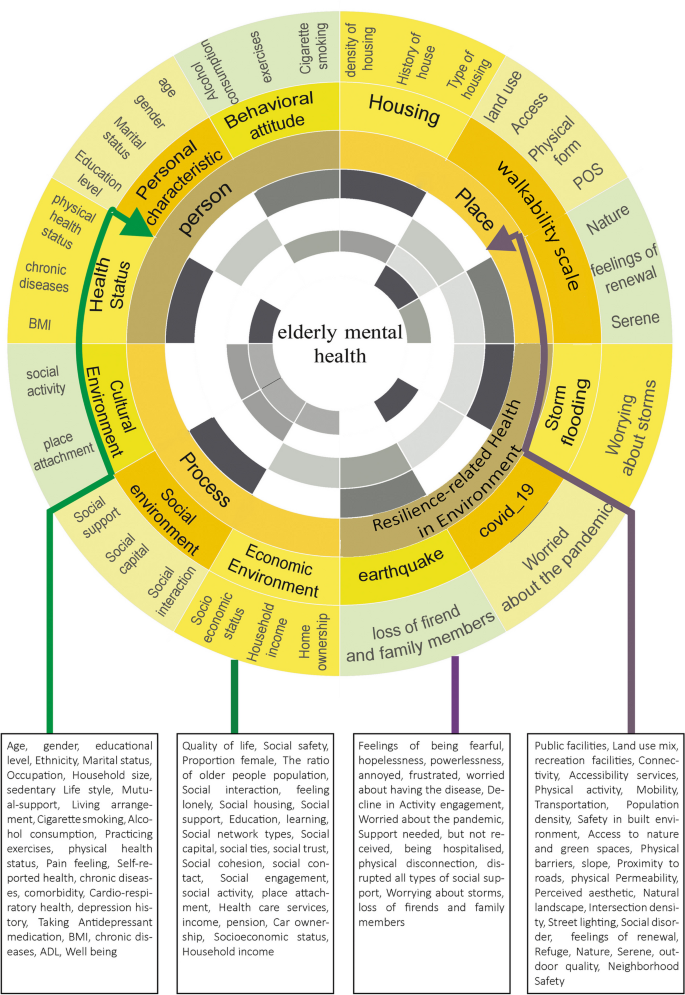
Results
Our finding mirrors four dimensions of creating healthy and sustainable environments for older adults: person, place, processes, and resilience-related health in the living environment. The person dimension includes individual characteristics, attitudes and behaviors, and health status. The place dimension is divided into five categories: land use, access, physical form, public open spaces, and housing, while the process consists of the social, cultural, and economic environments. Resilience-related health dimension emphasizes the impact of natural and man-made disasters on older people’s mental health.
Discussion
These findings can provide policymakers insights into developing community-based environmental intervention strategies to promote mental health among older adults and support healthy and active aging.
Background
There are more than 703 million older adults over age 65 worldwide. The increasing population of older people is caused by a decrease in the fertility rate and increasing life expectancy [1]. East and South-east Asia have the world’s largest aging adult population, with more than 260 million people, followed by Europe and North America, with more than 200 million people. By 2050, the older population will double to 1.5 billion [2]. Moreover, urban residents, that is, the people living in urban areas, comprise more than 55 percent of the world's population. Statistics predict that by 2050, more than 68% of the world's population will live in cities [3].
Moreover, the Organization for Economic Cooperation and Development (OECD) shows that the share of the population of people over 65 years old will increase to 25.1% in its member countries in 2050. Thus, cities particularly have many older residents, about 43.2% of the older adult population [4], indicating the coincidence of two significant phenomena of population aging and urbanization in the coming years. The Sustainable Development Goals (SDGs), developed by the United Nations, emphasize the health and well-being of all, especially older people [5]. The World Health Organization defines healthy aging as creating and sustaining functional capacity that leads to well-being in old age [6].
Recently, the mental health of older adults has been considered one of the significant issues that attracted the attention of researchers and policymakers. The World Health Organization (WHO) defines mental health as a state of well-being in which each person can realize their potential, cope with the stresses of life, work productively, and contribute to their community [7]. Hoisington et al. (2019) mentioned that Mental health includes emotional and social well-being components as well as social skills and cognitive functions affecting participation in basic tasks and social roles [8]. According to the Global Burden of Disease Survey (2015), depression and anxiety are the leading mental illnesses (ranked third and ninth, respectively) that cause the most problems worldwide, associated with various health problems, such as cardiovascular diseases and reduced quality of daily life, particularly among older people [9]. Older people’s mental health is becoming a growing public health concern [10].
Although national patterns of depression have been documented, research about older people has received less attention [11]. Specifically, neurological and psychiatric disorders account for 6.6% of all disabilities, the fifth leading cause of disease in the older population [12].
According to [13], with increased social participation among older adults, more time in physical activity, and more frequent contact with neighbors and children, their depression can be reduced [13]. Ko et al. 2019 believed that older men were significantly more likely to report feelings of loneliness, depression, and frequent suicidal thoughts than women. Older women were more likely to report higher stress levels and depressive symptoms. Older people who work suffer from more stress and, at the same time, experience fewer depressive symptoms [14].
Furthermore, the built environment is potentially involved in the mental disorders of older adults through its effects on social communication, access to green space, exposure to noise, traffic, or air pollution, and changes in individual behaviors, such as physical activity [15]. Evidence shows that the physical and social dimensions of the neighborhood environment play an essential role in older peoples’ health to predict health outcomes beyond individual deprivation and psychosocial characteristics [16]. For instance, according to research, older people living in pedestrian-friendly urban areas (with easier access to facilities, beautiful scenery, open spaces, and road safety) are generally more physically active and healthier [17]. Furthermore, older adults are more vulnerable to stressors or risks due to reduced physical performance against environmental barriers [18]. Compared to younger adults, older adults appear to be more vulnerable to changes in the built environment [19].
Today, urban resilience is considered a paradigm affecting all aspects of human life. Meerow (2016) proposed a new definition for urban resilience be defined as the following: “Urban resilience refers to the ability of an urban system and all its constituent socio-ecological and socio-technical networks across temporal and spatial scales to maintain or rapidly return to desired functions in the face of a disturbance, to adapt to change, and to quickly transform systems that limit current or future adaptive capacity [20]”. They added socio-economic dynamics such as public health, monetary capital, demographics, and Justice and equity to shape the other subsystems. The livelihoods and capacities of urban citizens have a significant role in enhancing urban resilience. Furthermore, after the COVID-19 outbreak, urban resilience is critical to urban and human health. Resilience is the capacity of a system or community at risk to withstand, adapt to, and recover from the effects of a hazard in a timely and effective manner [21].
The COVID-19 outbreak caused the disconnection of older adults from the outdoor environment, and older people with a history of depression reported higher levels of depression or sadness during the pandemic [22]. Fear of being infected with the virus, hospitalization of family members, disconnection of the senior from social support, and fear of losing a job can also affect older people’s mental health [22,23,24]. Although some studies show that younger people were more emotionally involved than seniors in disasters such as the COVID-19 pandemic, others show that older people suffer a more significant threat and death from catastrophes. Additionally, some authors have discovered a relationship between emotional well-being, resilience, and social support among caregivers exposed to social isolation [25].
In recent years, many studies have measured the impact of social, economic, health, individual, and demographic factors on the mental health of older adults; however, there is still no comprehensive model for measuring the factors affecting older adults' mental health in urban areas. This review study aims to find the factors affecting the mental health of older people living in urban environments by reviewing papers published in the last seven years by focusing on understanding the general determinants of older people’s mental health in the cities as a narrative systematic review. This study provides a deep understanding of the factors affecting the mental health of older adults for policymakers to make plans to increase the mental resilience of older adults and improve their quality of life.
Methods
A scoping review is a good tool for identifying domains or covering a body of literature on a particular topic, identifying knowledge gaps, existing literature, and concepts [26]. Arksey and O’Malley used a systematic scoping review for the first time in five main steps: identifying research questions, identifying related studies, selecting studies, charting and collecting data, and summarizing and reporting research results [27]. This method was then improved by Daudt et al. 2013, Levac et al. 2010, and Colquhoun et al. 2014 [28,29,30]. This study followed the PRISMA extension for scoping reviews (PRISMA-SCR) [31]. In recent years, some studies have been conducted on older people's mental health, each focusing on specific dimensions. Due to the complex nature of mental health, the scoping review is used in this study to identify knowledge gaps and reveal various factors affecting older people’s mental health.
Identifying research questions
The first step in the scoping review is to identify research questions to reveal and link them to the research objectives. This study aims to review the papers on the mental health of older adults to identify the factors that can affect the mental health of older adults living in the urban environment in the face of stressful aspects (conditions such as COVID-19) and lead to an increase in urban resilience among older people. For this purpose, the following questions have been used to refine the research.
-
1-
What factors affect Older adults’ mental health living in urban environments?
-
2-
What factors affect Older adults’ mental health living in the city In facing disasters and changes, ‘for instance, COVID-19’, to achieve urban resilience?
Identify related studies
We searched Scopus, PubMed, Web of Science, and Google Scholar for relevant papers from 2015 to 10 May 2022. Search strategies drafted by a professional person and refined through team discussion. The search terms were “mental health” and / OR “neighborhood” and / OR “urban area”, and “environment” and / OR “older people” and / OR “social environment” and / OR “built environment” and / OR “depression” and “anxiety” and “stress” and “Covid -19”. Article in Press in Scopus Database, Rural context-based, and non-English papers were excluded.
Selection of studies
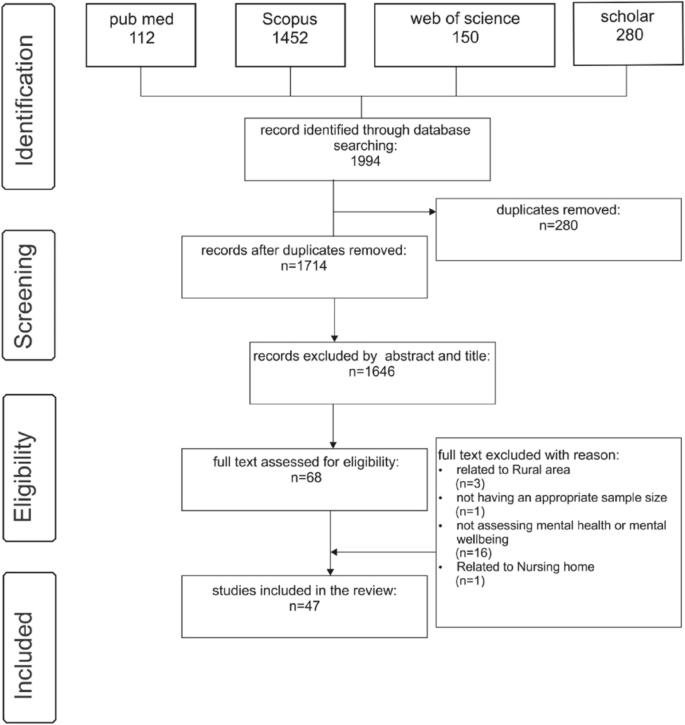
One thousand nine hundred ninety-four papers were collected after searching the databases. First, 280 duplicate papers were removed, and then, based on the analysis of abstracts and titles, 1646 other papers were removed from the study. After a complete review of the papers, 21 were removed from the list due to their relevance to the rural environment, lack of suitable sample sizes, failure to calculate mental health or mental well-being, and relevance to nursing homes. To increase consistency among reviewers, All reviewers screened the first 60 publications and discussed the review’s screening and result.
Three authors did the initial review of the abstracts and titles, and after reviewing, all authors decided which paper would remain for further study. After this process, 47 papers complied with the criteria. It should be mentioned that 4 of the documents were review papers. The article selection process, the PRISMA process, is presented in Fig. 1.
Charting and interpreting data
For data extraction and charting, this study follows [28, 30] recommendations for scoping review data extraction and charting. In this regard, the authors chose the narrative review approach for data charting, as described in [30]. Based on this, Two reviewers developed an Excel file to examine which data needs to be extracted. Then, all related data were collected in an Excel file after selecting the papers. The Data included authors, year, geographical location, research scale, method, mental health measurement tool, personal factors, health factors, physical environment factors, social environment factors, economic factors, age of participants, and key findings.
Collecting, summarizing, and reporting the results
The last stage of the scoping review is collecting, summarizing, and reporting the results. Thematic analysis was used to combine, categorize, and codify the studies’ findings regarding the research questions and aims. Thematic analysis of the papers was done with an emphasis on the factors affecting older people’s mental health, such as the dimensions of the built environment, social environment, individual characteristics, and health status. Table 1 presents the categorizing process used in data analysis and coding.
Results
Table 2 shows the characteristics of the reviewed papers. Twenty-seven studies (57.4%) are from Asia, ten studies (21.3%) are from Europe, and six studies (12.8%) are from America. In addition, the most significant number of studies is related to the Chinese mainland, with 11 (21.4%) studies, and Hong Kong, China, with eight studies (17%). Also, 41 (87.23 percent) studies were conducted with the quantitative method and 2 (4.25) with the qualitative approach. Four studies are review articles.
Analysis of assessment tools of mental health consisting of CES-D (n = 11) and GDS-15 (n = 9) was used in these studies to measure older adults' mental health. Tools such as HADS, UCLA, MSC, SF-12, SF-36, PSS, MMSE-2SV, SWLS, and GAI were also employed. Table 3 shows the mental health measurement tools used in the papers.
Older people studied in the papers were generally aged 60 and over (41.2 percent) and 65 and over (32.3 percent). Additionally, more than 74% of the studies mirror the environment dimension and its impact on mental health, as 46% examined the effects of the social environment on the mental health of older adults. In 14 papers, the impact of economic factors on older people’s mental health was studied; however, 46% of the papers considered personal health and its role in mental health. 46% of studies examined personal characteristics and their effect on mental health. Ten studies considered factors such as physical activity, social activity, the proportion of older people population, social relationships, household income, and social capital as mediating factors affecting older people’s mental health. Three papers examined the cultural aspects and their impact on mental health, and five studied the social health of older people against disasters, especially the COVID-19 virus. The main dimensions and codes are summarized in Fig. 2.
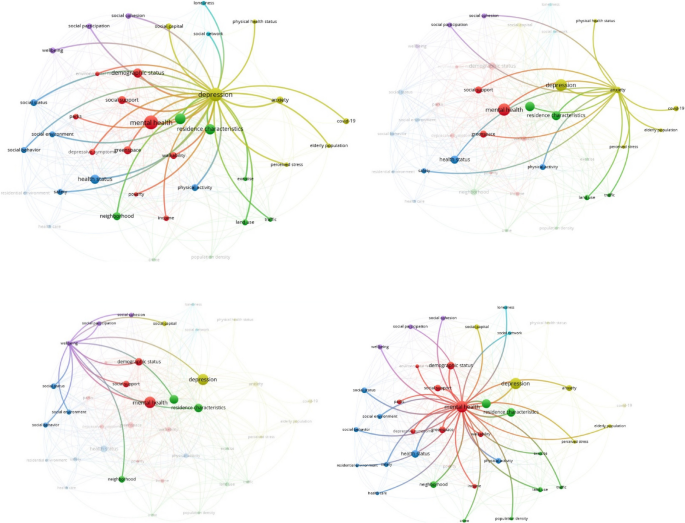
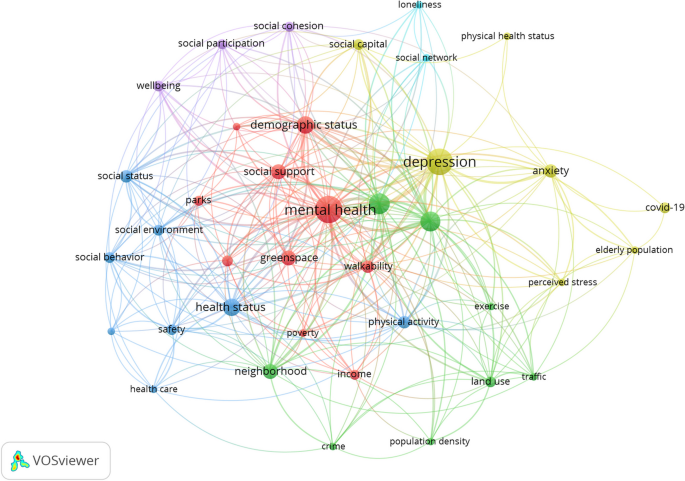
According to the findings, intricate interactions between factors were investigated through the Co-occurrence of keywords with VOS Viewer for four mental health disorders reviewed in this study: mental health, well-being, anxiety, and depression. Each of these shows the different relationship between mental health and environmental determinants. Mental health factors include social support, social cohesion, social network, social capital, social status, land use, traffic, Healthcare, crime, income, health status, social environment, social behavior, residence characteristics, exercise, population density, green space and parks, residential environment, safety, neighborhood, perceived stress, demographic status, older adults population. Figure 3 shows the network visualization map.
Well-being is linked to social participation, cohesion, social support, social capital, demographic status, residence characteristics, social environment, and social behavior. Depression disorder is related to physical health status, walkability, health status, safety, income, neighborhood, physical activity, safety, land use, traffic, residence characteristics, green space and parks, social participation, social cohesion, social support, social capital, social network, demographic status, loneliness, poverty, neighborhood, social status. Anxiety disorder is connected to social support, social participation, social cohesion, residence characteristics, physical activity, older adult population, health status, land use, traffic, green space, COVID-19 outbreak, perceived stress, and safety. Additionally, as shown in the Co-occurrence term, depression highly impacts older people’s mental health.
The above findings explain that the various dimensions of mental health in older people are most influenced by environmental, individual, social, personal health, and economic factors. The paper’s review showed that older people’s mental health was associated with many factors, including the built and social environment. After thoroughly reviewing the papers, the factors affecting older people’s mental health were identified, and concepts related to various environmental dimensions were coded. The dimensions and criteria based on the Vos viewer are presented in Fig. 4.
Personal dimension
This dimension includes three sub-dimensions: personal characteristics, attitudes and behaviors, and health status. The following criteria and definitions of individual determinants have been extracted and coded from 32 papers. The papers have considered personal factors such as age, gender, education level, ethnicity, race, house ownership, employment, marriage, household size, sedentary lifestyle, mutual support, and living arrangement [32,33,34,35]. Three studies reported that living in areas with a high percentage of older people directly impacted older people’s health. Domènech-Abella et al. (2020) stated that a sedentary lifestyle and less physical activity reduce older people’s mental health. Attitudes and behaviors comprise three components: smoking, alcohol consumption, and physical exercise [13, 14, 36]. Byeon (2019) showed that older people who do flexibility exercises for an average of 1 to 4 days are 81 percent less likely to develop depression than those who do not. People who smoke are more likely to experience high-stress levels and depression [14].
Lam et al. (2020) showed a close relationship between personal characteristics such as physical and body weight and mental health. Moreover, individual health factors include physical health, well-being, pain sensation, functional ability, self-assessment of health, body mass index (BMI), restrictions on daily activities, chronic diseases, co-occurrence of multiple disorders, and lung diseases [31, 35, 39, 47]. Therefore, people with a good BMI will be healthier and experience better mental health. Also, having two or more diseases simultaneously affects mental health [14].
Place-based dimension
The place dimension can affect older people’s mental health to a large extent, which is presented in 35 studies. The place-based features include land use, access, physical form, public open spaces, and housing. Eleven studies focused on land use, including proximity to services, public facilities, land use mix, and sports facilities [34, 37]. Koohsari et al. (2019) report that women with better access to transportation stations have a higher level of mental health. Commercial and recreational facilities directly impact the mental health of older adults. The access factor is considered in 13 studies and includes connectivity, service access, mobility, pedestrian environment, and public transportation [38,39,40]. Low walkability of the built environment increases the chances of loneliness, which is associated with mental health [37].
Additionally, physical form, which was considered in 14 studies, includes population density, safety, access to green space, physical barriers, slope and topography, proximity to roads, physical permeability, familiarity with the environment, Environmental aesthetics, natural landscapes, and residential density [41,42,43]. Perception of safety is related to the physical and mental health of older people [44]. Furthermore, decreasing physical barriers and crime in the neighborhood increase older people’s mental health [18]. Public open space was considered in 13 papers, paying attention to issues such as street lighting, safety against crime, social disorders, availability of water spaces, recreational spaces, environmental cleanliness, noise pollution, congestion, Landscapes, outdoor quality, green and blue space coverage, restoration Serene, nature restoration, social restoration, landscape, restoration refuge and a sense of renewal [41, 45, 46].
More importantly, public open spaces significantly impact older people’s mental health, so green and blue infrastructures in the neighborhood and near beaches and lakes are associated with reduced use of antidepressants [10]. Green spaces are also associated with increased physical activity, improving mental health perception and well-being, and promoting older people’s mental health [34, 47]. Ten papers consider housing quality, neighborhood safety, housing density, housing facilities, type of housing, length of stay, interior design, and house history [38, 48, 49]. The quality of housing and the neighborhood’s safety affect older adults' mental, physical, and mental health [50]. External building characteristics, interior design, home facilities, and interior home space profoundly impact the mental health of older people [49].
Procedural determinants
Procedural dimensions include social, cultural, and economic environments. The social environment affects the mental health of older adults in various ways. Chen et al. (2016) stated that older people, with the support of friends or family, have better mental health; additionally, social capital can play a supportive role in mental health [27]. The essential components of the social environment are presented in 21 papers, including quality of life and health, social safety, the ratio of women in the neighborhood, the ratio of older people population in the neighborhood, social interactions, feeling lonely, social housing, social support, education, learning, social network type, different types of social capital, Social nodes, trust, and social cohesion [34, 38, 51, 55].
Besides, the cultural environment was repeated in three papers. Older people’s participation in social activities reduces stress and depression in older people [14]. This sub-theme profoundly affects the mental health of older adults and includes two criteria for social activities: the sense of place and identity [51, 52].
According to our review, social and economic status is the most critical component of the economic factor. The economic environment is studied in 15 papers related to health: income/retirement, socio-economic status, car ownership, housing ownership, and household income [42, 53, 54].
Resilience-related health in environment dimension
Natural disasters and crises profoundly affect mental health. Five papers specifically address the issue of Covid-19 and its impact on older adults’ social health and resilience. With the Coronavirus outbreak, many older people were forced to stay home. Lockdowns and cocoons caused some problems profoundly affecting older people’s mental health. Dimensions introduced in these studies include cases of being affected by COVID-19, feeling lonely, fear, despair, helplessness and fatigue, fear of getting COVID-19, decreased participation in activities, need to receive support, frequent communication with others, hospitalization, disconnection, and loss of social support [23, 24, 55]. Older people’s physical activity has significantly decreased during the pandemic; thus, the severity of depression in women has increased [56]. Two studies have examined the impact of disasters on mental health, which refer to the fear of storms and the loss of families, respectively [57, 58].
Discussion
This study has used a scoping review to identify, select, and combine the findings of studies that have examined determinants affecting the mental health of older adults in urban areas in the context of urban resilience. We found that urban resilience refers to a city’s capacity to support its citizens and systems. Like humans, cities are resilient due to a variety of intricate variables. Surprisingly, however, there is a conceptual link between urban and psychological resilience because both ultimately benefit the person or citizen. As a result, the elements that contribute to urban resilience may also contribute to mental resilience and vice versa.
As a result, the conceptual similarity between urban and psychological resilience is rational, and the distinct characteristics that distinguish the two are likewise connected. Researching these elements and looking at resilience’s impact on mental health in urban settings would be fascinating. Based on reviewing the previous paper, we introduce the ideas of older adults’ mental health and urban resilience, describe urban resilience's functional link with older adults’ mental health, and pinpoint the characteristics of urban resilience in four dimensions of determinants associated with mental health in older people (anxiety, depression, mental health, and well-being), including personal and place-based factors, processes in the living environment (social, cultural, and economic), and environmental health (natural and man-made disasters).
Urban Resilience focuses on the system’s ability to maintain environmental harmony despite perturbations. Additionally, it aids in the recovery of individuals from disturbance. It deals with the capacity to adjust to and respond to structural change throughout time. Thus, most studies have pointed out the effect of older people’s characteristics on their mental health as the most influential factor. Regarding socio-economic processes, studies have emphasized the role of social capital, social interactions, perception of social security, and the economic status of older people in improving their mental health of the older people. This study scrutinizes the mental health of older adults by analyzing the geographical scope, tools for measuring older people's mental health, and key findings on the main reported determinants of older people’s mental health to provide comprehensive knowledge about the consequences of the results and gaps which can be helpful for physicians, researchers, and aging policymakers.
Based on the role of urban structure and place in building urban resilience, the place and land use range mix has been found in most studies. Still, some individual variables that refer to walkability in these studies (such as crosswalks, barrier-free sidewalks, and recreational environments) have a significant relationship with health. In particular, the presence of green space/park was the most studied variable in all areas related to mental health outcomes. A few studies paid attention to individual and place-based determinants. In contrast, the qualitative studies paid more attention to the perceptual characteristics of the quality of housing, the perception of environmental security, and the perception of the social environment.
In addition, perceptions of environmental health, fear of infectious diseases such as COVID-19, and injuries caused by natural and man-made disasters were considered in the papers. Most studies that looked at the impact of individual and environmental factors on older people’s mental health found significant relationships, with evidence supporting the moderating effects of demographic characteristics, health status, health behaviors, neighborhood walkability, and an area’s level of development intensity. The mediating results of both personal and place-based dimensions were not confirmed. Due to significant differences in research methodology, measurement methods, sample sizes, and neighborhood definition, direct comparisons between studies are impossible.
In addition, the results of the analysis of the keywords in VOS viewer showed that the study of factors such as Demographic Status, Health status, Social support, Green space, Walkability, Neighborhood Characteristics, Physical activity, Social Support, Social environment in research related to mental health is of great importance and has been studied more than the rest of the factors. Also, some factors such as traffic safety, safety, exercise, loneliness, social network, and physical health status have been less discussed.
Methodological limitations of review studies
A- Lack of standard tools in measuring the determinants of mental health: Contradictory findings on the role of the four dimensions on older people’s mental health may be partly due to the lack of clarity in the definition of standard mental health measurement tools for the four dimensions of individual, place, process, and environmental health. This problem is the most prevalent in place-based features, which mention various tools to study the effects of place-based features on older people’s mental health. Other studies have pointed to the lack of standard tools in investigating the factors affecting older people’s mental health [59]. Studies such as Ivey et al. (2015) point to using common mental health tools to link mental health and neighborhood measurement metrics using various data [44].
b- Lack of evaluation of specific Place-based features: Most Place-based features studied in the papers, such as public parks, access to public transportation, and land use composition, are among the common features necessary for healthy aging. Although an increasing number of studies have studied the separated criteria instead of integrated criteria to portray the role of individual and Place-based components, there is still a knowledge gap about place-based features that may affect the mental health of older adults. A small amount of literature outside the scope of this study, including unreviewed documents, suggests potential design solutions for adapting outdoor environments to mental health. They consider some design dimensions such as distinctive architectural features, ample street facilities (such as shaded chairs and lighting), a clear hierarchy of locations, comprehensive, simple, unobstructed sidewalks, and short and distinctive pedestrian crossings. These place-based features are attractive targets for interventions because they are generally more practical and sustainable than large-scale environmental or program-based interventions. Future studies need to identify valid and consistent ways to measure the role of specific design features and establish more robust paths between place-based characteristics and older people’s mental health. For example, green space is an essential Place-based feature playing a significant role in promoting the health of older people, particularly mental health [60]. However, our findings indicate that the total area/ratio of green space alone may not fully show a significant impact on health outcomes, and future research should consider the morphology and quality of green space for better assessment. There are no specific measuring tools for housing quality for older people, especially social housing. Studies conducted in this regard examined the needs and preferences of older adults and their effect on older people's mental health using qualitative methods.
Assessing the mental health of the older people
Mental health in older people has several definitions. Studies considered mental health in older adults as cognitive health; consequently, the loss of mental health is considered dementia in older people [59]. Another range of studies related to mental health emphasized some emotions such as stress, depression, and anxiety [15, 34, 43, 56, 61, 62]. Despite different emotions in older people, there was no standard and comprehensive tool for mental health testing in older people. The most used tools were CES-D and GDS-15, which were used to study the rate of depression in older adults, and the others, the emotional disorders, in older adults received little attention. Especially when health is endangered in conditions such as pandemics or natural hazards, these instruments have little efficiency in measuring older people’s mental health, and most studies have turned to qualitative studies.
Study of mediating effects
Five studies looked at mediators focused on P.A. or walking outcomes using subjective self-reports, and three used objective measures (accelerometer measure of P.A.). In some papers, the mediating effects of subjectively estimated P.A. or walking were considerable. As respondents may not recall their previous physical activity accurately, this assessment approach frequently results in recall bias, limiting the capacity to find reliable relationships with cognitive function. Future studies should use objective techniques to capture P.A. levels more accurately and prove its mediation function in mental health conditions. Furthermore, more research is needed to understand the underlying mechanism of the long-term link between greenness and mental health. Depression was also discovered to mediate the relationship between urbanization and personal/crime-related safety [41].
In recent years, cities in North Africa and the Middle East have been experiencing special conditions under the influence of climatic phenomena. Every year, many people die due to dust. The vulnerable groups suffering from these changes are older people, who have to stay home because of the effects of these factors on health. Prolonged stay at home and disconnection from the external environment have affected older people’s mental health, so it is suggested that future research consider the effects of dust and climate change on older people’s mental health.
Strengths and limitations of the research
This research uses a scoping review method and a systematic search strategy based on research questions. In this study, a selection of scientific evidence and studies conducted on the mental health of older adults living in the city can be used to strengthen older people’s mental health in cities. This study also facilitates the formation of future research with a comprehensive view and by identifying different dimensions of mental health in older people. There are several limitations to the scoping review in this study. First, In this research, only four databases in English have been examined, which means that studies from other languages have not been included. Second, this study did not investigate factors such as dementia, schizophrenia, bipolar disorder, cognitive disorders, and suicide related to mental health disorders in older adults. Third, in this study, only research with the urban context is considered, and older people living in rural areas are out of the scope of this research. Fourth, different dimensions of the impact of the COVID-19 pandemic on the mental health of older people under environmental health are presented in this study. We suggest that in future research, the effect of the COVID-19 pandemic on the mental health of older adults living in cities be examined in more depth. Fifth, the significant studies included in this study are from developed countries in Asia, Europe, and America, so the findings of this study may be less applicable in developing countries. Sixth, Some natural disasters, such as floods and earthquakes, have not been investigated in this study. Still, since these factors affect the mental health of older people in resilient environments and there is a need to study in this field, some of the effects of these factors are shown in 5 4 to emphasize this issue. Only two factors were considered influential factors in mental health to highlight the importance of catastrophe on older people’s mental health. It is suggested that these factors’ role in older people’s mental health be examined in more detail in future research.
Conclusion
This study has presented a comprehensive and valid review of the papers about determinants of mental health of older adults in the context of the urban resilience approach that has been of interest in recent years. In this study, urban resilience is defined as the ability of the urban environment and its residents to maintain continuity in the face of shocks and stresses, especially for vulnerable older adults, so that they can adapt positively to achieve a sustainable environment. The results of this study have been presented in the form of a conceptual model that refers to the cognitive health component of older people, including personal and spatial dimensions, socio-economic and cultural processes, and health-oriented environments. The personal dimension refers to older adults’ demographic characteristics, health behaviors, and health status. The spatial dimension relates to land use, access, urban form, urban space, and the quality of older people’s neighborhoods.
Procedural components examine socio-cultural processes, economic conditions, and the policy-making and governance environment (including urban and health management). The difference between this study’s results and cognitive health components is the resilience-related health component, which tries to increase the adaptability of older adults in the face of shocks and disasters, including natural disasters and shocks caused by future infectious diseases that have affected the urban older people community during COVID-19. These components can make it possible to realize urban resilience with resilient residents.
Future related studies in designing a healthy and resilient environment for older people in a situation where climate changes, fine dust, and various phenomena resulting from global warming affect cities can effectively promote older people’s health and ultimately improve older adults’ health. The findings of this review can also provide insights for policymakers and those involved in planning and designing the development of environmental intervention strategies at the community level to promote mental health and resilience among older people and support healthy and active aging.
Availability of data and materials
After request, supporting data and data analysis materials are available from the corresponding author (AZ).
References
United Nations Department of Economic and Social Affairs PD. World Population Ageing 2020 Highlights: Living arrangements of older persons. In. United Nations Publication; 2020.
Nations U. World Population Ageing 2019 Highlights. United Nations; 2019.
Nations U. World Urbanization Prospects: The 2018 Revision. United Nations; 2018.
OECD. Ageing in Cities. In. Paris; 2015.
Pandey NM, Tripathi RK, Kar SK, Vidya K, Singh N. Mental health promotion for elderly populations in World Health Organization South-East Asia Region: Needs and resource gaps. World J Psychiatry. 2022;12(1):117.
Tavares RE, Jesus MC, Machado DR, Braga VAS, Tocantins FR, Merighi MAB. Healthy aging from the perspective of the elderly: an integrative review. Revista Brasileira de Geriatria e Gerontologia. 2017;20:878–89.
WHO. Promoting mental health : concepts, emerging evidence, practice : summary report / a report from the World Health Organization, Department of Mental Health and Substance Abuse in collaboration with the Victorian Health Promotion Foundation and the University of Melbourne. Geneva: World Health Organization; 2004.
Hoisington AJ, Stearns-Yoder KA, Schuldt SJ, Beemer CJ, Maestre JP, Kinney KA, Postolache TT, Lowry CA, Brenner LA. Ten questions concerning the built environment and mental health. Build Environ. 2019;155:58–69.
Wang R, Liu Y, Lu Y, Zhang J, Liu P, Yao Y, Grekousis G. Perceptions of built environment and health outcomes for older Chinese in Beijing: A big data approach with street view images and deep learning technique. Comp Environ Urban Syst. 2019;78:101386.
McDougall CW, Hanley N, Quilliam RS, Bartie PJ, Robertson T, Griffiths M, Oliver DM. Neighbourhood blue space and mental health: A nationwide ecological study of antidepressant medication prescribed to older adults. Landsc Urban Plan. 2021;214:104132.
Yang KH, Han BH, Moore AA, Palamar JJ. Trends in major depressive episodes and mental health treatment among older adults in the United States, 2010–2019. J Affect Disord. 2022;318:299–303.
Arias-Fernández L, Carcedo-Argüelles L, Martín-Payo R, López-García E, Rodríguez-Artalejo F, Lana A. Association between neighborhood physical characteristics and mental health among older adults in Spain. Geriatr Nurs. 2023;49:170–7.
Wang R, Feng Z, Liu Y, Lu Y. Relationship between neighbourhood social participation and depression among older adults: A longitudinal study in China. Health Soc Care Community. 2020;28(1):247–59.
Lee HJ, Lee DK. Do sociodemographic factors and urban green space affect mental health outcomes among the urban elderly population? Int J Environ Res Public Health. 2019;16(5):789.
Pun VC, Manjourides J, Suh HH. Close proximity to roadway and urbanicity associated with mental ill-health in older adults. Sci Total Environ. 2019;658:854–60.
Toma A, Hamer M, Shankar A. Associations between neighborhood perceptions and mental well-being among older adults. Health Place. 2015;34:46–53.
Bhuyan MR, Yuen B. Older Adults’ Views of the Connections between Neighbourhood Built Environment and Health in Singapore. J Popul Ageing. 2022;15(1):279–99.
Zhao Y, Chung PK. Neighborhood environment walkability and health-related quality of life among older adults in Hong Kong. Arch Gerontol Geriatr. 2017;73:182–6.
Yue Y, Yang D, Owen N, Van Dyck D. The built environment and mental health among older adults in Dalian: The mediating role of perceived environmental attributes. Soc Sci Med. 2022;311:115333.
Meerow S, Newell JP, Stults M. Defining urban resilience: A review. Landsc Urban Plan. 2016;147:38–49.
Jha AK, Miner TW, Stanton-Geddes Z. Building urban resilience: principles, tools, and practice. World Bank Publications; 2013.
Paccagnella O, Pongiglione B. Depression deterioration of older adults during the first wave of the COVID-19 outbreak in Europe. Soc Sci Med. 2022;299:114828.
Khalaf OO, Abdalgeleel SA, Mostafa N. Fear of COVID-19 infection and its relation to depressive and anxiety symptoms among elderly population: online survey. MECP. 2022;29(1):7.
Sit RWS, Lai HHK, Dong D, Wang B, Wong MCS, Chung RYN, Wong SYS. Explaining the psychosocial effects of COVID-19 among older Hong Kong Chinese people—a qualitative analysis. J Geriatr Psychiatry Neurol. 2022;35(2):206–14.
Perez-Rojo G, López J, Noriega C, Velasco C, Carretero I, López-Frutos P, Galarraga L. A multidimensional approach to the resilience in older adults despite COVID-19. BMC Geriatr. 2022;22(1):793.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69.
Daudt HML, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol. 2013;13(1):48.
Colquhoun HL, Levac D, O’Brien KK, Straus S, Tricco AC, Perrier L, Kastner M, Moher D. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–4.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73.
Sohn SY, Joo WT, Kim WJ, Kim SJ, Youm Y, Kim HC, Park YR, Lee E. Social network types among older Korean adults: Associations with subjective health. Soc Sci Med. 2017;173:88–95.
Kabisch N, Püffel C, Masztalerz O, Hemmerling J, Kraemer R. Physiological and psychological effects of visits to different urban green and street environments in older people: A field experiment in a dense inner-city area. Landsc Urban Plan. 2021;207:103998.
Pun VC, Manjourides J, Suh HH. Association of neighborhood greenness with self-perceived stress, depression and anxiety symptoms in older U.S adults. Environ Health. 2018;17(1):39.
Guo Y, Liu Y, Lu S, Chan OF, Chui CHK, Lum TYS. Objective and perceived built environment, sense of community, and mental well-being in older adults in Hong Kong: A multilevel structural equation study. Landsc Urban Plan. 2021;209:104058.
Wang R, Liu Y, Xue D, Helbich M. Depressive symptoms among Chinese residents: how are the natural, built, and social environments correlated? BMC Public Health. 2019;19:1–8.
Domènech-Abella J, Mundó J, Leonardi M, Chatterji S, Tobiasz-Adamczyk B, Koskinen S, Ayuso-Mateos JL, Haro JM, Olaya B. Loneliness and depression among older European adults: The role of perceived neighborhood built environment. Health and Place. 2020;62:102280.
Khosravi H, Tehrani SO. Local Environment, Human Functions and the Elderly Depression and Anxiety. Ageing Int. 2019;44(2):170–88.
Lam WWY, Loo BPY, Mahendran R. Neighbourhood environment and depressive symptoms among the elderly in Hong Kong and Singapore. Int J Health Geogr. 2020;19(1):48.
Tang S, Lee HF, Feng J. Social capital, built environment and mental health: A comparison between the local elderly people and the “laopiao” in urban China. Ageing Soc. 2022;42(1):179–203.
Barnett A, Zhang CJ, Johnston JM, Cerin E. Relationships between the neighborhood environment and depression in older adults: a systematic review and meta-analysis. Int Psychogeriatr. 2018;30(8):1153–76.
Gan DRY. Neighborhood effects for aging in place: a transdisciplinary framework toward health-promoting settings. Hous Soc. 2017;44(1–2):79–113.
Koohsari MJ, McCormack GR, Nakaya T, Shibata A, Ishii K, Yasunaga A, Hanibuchi T, Oka K. Urban design and Japanese older adults’ depressive symptoms. Cities. 2019;87:166–73.
Ivey SL, Kealey M, Kurtovich E, Hunter RH, Prohaska TR, Bayles CM, Satariano WA. Neighborhood characteristics and depressive symptoms in an older population. Aging Ment Health. 2015;19(8):713–22.
Finlay J, Franke T, McKay H, Sims-Gould J. Therapeutic landscapes and well-being in later life: Impacts of blue and green spaces for older adults. Health Place. 2015;34:97–106.
Qiu L, Chen Q, Gao T. The effects of urban natural environments on preference and self-reported psychological restoration of the elderly. Int J Environ Res Public Health. 2021;18(2):1–14.
Abraham Cottagiri S, Villeneuve PJ, Raina P, Griffith LE, Rainham D, Dales R, Peters CE, Ross NA, Crouse DL. Increased urban greenness associated with improved mental health among middle-aged and older adults of the Canadian Longitudinal Study on Aging (CLSA). Environ Res. 2022;206:112587.
Domènech-Abella J, Switsers L, Mundó J, Dierckx E, Dury S, De Donder L. The association between perceived social and physical environment and mental health among older adults: mediating effects of loneliness. Aging Ment Health. 2021;25(5):962–8.
Li C, Zhou Y. Residential environment and depressive symptoms among Chinese middle- and old-aged adults: A longitudinal population-based study. Health Place. 2020;66:102463.
Liu Y, Dijst M, Faber J, Geertman S, Cui C. Healthy urban living: Residential environment and health of older adults in Shanghai. Health Place. 2017;47:80–9.
Hanslmaier M, Peter A, Kaiser B. Vulnerability and fear of crime among elderly citizens: what roles do neighborhood and health play? J Housing Built Environ. 2018;33(4):575–90.
Lu S, Liu Y, Guo Y, Ho HC, Song Y, Cheng W, Chui C, Chan OF, Webster C, Chiu RLH, et al. Neighborhood built environment and late-life depression: A multilevel path analysis in a Chinese society. J Gerontol B Psychol Sci Soc Sci. 2021;76(10):2143–54.
Curl A, Mason P. Neighbourhood perceptions and older adults’ well-being: Does walking explain the relationship in deprived urban communities? Transp Res Part A Policy Pract. 2019;123:119–29.
Mao S, Lu N, Xiao C. Perceived neighborhood environment and depressive symptoms among older adults living in Urban China: The mediator role of social capital. Health Soc Care Community. 2021.
Van Tilburg TG, Steinmetz S, Stolte E, van der Roest H, de Vries DH. Loneliness and mental health during the COVID-19 pandemic: A study among Dutch older adults. J Gerontol Series B. 2021;76(7):e249–55.
Li Y, Su S, Luo B, Wang J, Liao S. Physical activity and depressive symptoms among community-dwelling older adults in the COVID-19 pandemic era: A three-wave cross-lagged study. Int J Disaster Risk Reduct. 2022;70:102793.
Sirey JA, Berman J, Halkett A, Giunta N, Kerrigan J, Raeifar E, Artis A, Banerjee S, Raue PJ. Storm Impact and Depression Among Older Adults Living in Hurricane Sandy-Affected Areas. Disaster Med Public Health Prep. 2017;11(1):97–109.
Tsuboya T, Aida J, Hikichi H, Subramanian SV, Kondo K, Osaka K, Kawachi I. Predictors of depressive symptoms following the Great East Japan earthquake: A prospective study. Soc Sci Med. 2016;161:47–54.
Chen E, Wood D, Ysseldyk R. Online Social Networking and Mental Health among Older Adults: A Scoping Review. Can J Aging. 2022;41(1):26–39.
Lak A, Rashidghalam P, Myint PK, Baradaran HR. Comprehensive 5P framework for active aging using the ecological approach: an iterative systematic review. BMC Public Health. 2020;20(1):33.
Guo Y, Chang SS, Chan CH, Chang Q, Hsu CY, Yip PSF. Association of neighbourhood social and physical attributes with depression in older adults in Hong Kong: A multilevel analysis. J Epidemiol Community Health. 2020;74(2):120–9.
Ko H, Park YH, Cho B, Lim KC, Chang SJ, Yi YM, Noh EY, Ryu SI. Gender differences in health status, quality of life, and community service needs of older adults living alone. Arch Gerontol Geriatr. 2019;83:239–45.
Ruiz M, Scholes S, Bobak M. Perceived neighbourhood social cohesion and depressive symptom trajectories in older adults: a 12-year prospective cohort study. Soc Psychiatry Psychiatr Epidemiol. 2018;53(10):1081–90.
Wang R, Lu Y, Zhang J, Liu P, Yao Y, Liu Y. The relationship between visual enclosure for neighbourhood street walkability and elders’ mental health in China: Using street view images. J Transp Health. 2019;13:90–102.
Liu Y, Lu S, Guo Y, Ho HC, Song Y, Cheng W, Chui CHK, Chan OF, Chiu RLH, Webster C, et al. Longitudinal associations between neighbourhood physical environments and depressive symptoms of older adults in Hong Kong: The moderating effects of terrain slope and declining functional abilities. Health Place. 2021;70:102585.
Cho S. Relationships between perceived neighborhood disorder and depressive symptomatology: the stress buffering effects of social support among older adults. Soc Work Public Health. 2022;37(1):45–56.
Tan TH. Perceived environmental attributes: their impact on older adults’ mental health in Malaysia. Int J Environ Res Public Health. 2022;19(6):3595.
Byeon H. Relationship between physical activity level and depression of elderly people living alone. Int J Environ Res Public Health. 2019;16(20):4051.
Chen YY, Wong GHY, Lum TY, Lou VWQ, Ho AHY, Luo H, Tong TLW. Neighborhood support network, perceived proximity to community facilities and depressive symptoms among low socio-economic status Chinese elders. Aging Ment Health. 2016;20(4):423–31.
Won J, Lee C, Forjuoh SN, Ory MG. Neighborhood safety factors associated with older adults’ health-related outcomes: A systematic literature review. Soc Sci Med. 2016;165:177–86.
Friesinger JG, Topor A, Bøe TD, Larsen IB. Studies regarding supported housing and the built environment for people with mental health problems: A mixed-methods literature review. Health Place. 2019;57:44–53.
Miao J, Wu X, Sun X. Neighborhood, social cohesion, and the Elderly’s depression in Shanghai. Soc Sci Med. 2019;229:134–43.
Acknowledgements
Not applicable.
Funding
This study hasn’t used any funding support.
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: study conception and design: S.Vahabi and A.Lak.; data collection: S. Vahabi N. Panahi; analysis and interpretation of results: A.lak and S.Vahabi; draft manuscript preparation: S.Vahabi and A.Lak and N. Panahi. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table 1.
Reviewed article characteristics.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Vahabi, S., Lak, A. & Panahi, N. Driving the determinants of older people’s mental health in the context of urban resilience: a scoping review. BMC Geriatr 23, 711 (2023). https://doi.org/10.1186/s12877-023-04387-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04387-y