- Research
- Open access
- Published:
The impact of long-term care interventions on healthcare utilisation among older persons: a scoping review of reviews
BMC Geriatrics volume 24, Article number: 484 (2024)
Abstract
Background
As the ageing population grows, the demand for long-term care (LTC) services will rise, concurrently amplifying healthcare utilisation. This review aims to examine and consolidate information on LTC interventions that influence healthcare utilisation among older persons.
Methods
A scoping review was performed through a systematic search in PubMed, EBSCO CINAHL, EBM Reviews - Cochrane Database of Systematic Reviews, Embase, APA PsycInfo, EBM Reviews - Health Technology Assessment, and EBM Reviews - NHS Economic Evaluation Database. Systematic reviews with meta-analyses published between 1 January 2010 and 2 June 2022 among older persons aged 60 and above were included. The characteristics of LTC interventions were mapped to the World Health Organization (WHO) Healthy Ageing Framework. The effect sizes of healthcare utilisations for LTC interventions were recalculated using a random-effects model. The methodological quality was assessed with the AMSTAR-2 checklist, while the quality of evidence for each association was evaluated using GRADE.
Results
Thirty-seven meta-analyses were included. The most prominent domain of the healthy ageing framework was managing chronic conditions. One hundred twelve associations between various LTC interventions and healthcare utilisations were identified, with 22 associations impacting healthcare utilisation. Four interventions were supported by suggestive or convincing evidence. Preventive home visits were found to reduce hospital admission (OR: 0.73, 95% CI: 0.59, 0.91, p = 0.005), caregiver integration during discharge planning (OR: 0.68, 95% CI: 0.57, 0.81, p < 0.001), and continuity of care (OR: 0.76, 95% CI: 0.61, 0.95, p = 0.018) reduced hospital readmission, and perioperative geriatric interventions reduced the length of hospital stay (MD: -1.50, 95% CI: -2.24, -0.76, p < 0.001). None of the associations impacted emergency department visits, medication use, and primary care utilisations with convincing evidence. Most reviews received low methodological quality.
Conclusion
The findings suggest that LTC interventions could benefit from transitioning to a community-based setting involving a multidisciplinary team, including carers. The spectrum of services should incorporate a comprehensive assessment to ensure continuous care.
Background
Population ageing is a global phenomenon, with the number of older persons projected to double from 771 million in 2022 to 1.6 billion in 2050 [1]. Low—and middle-income countries (LMICs) are projected to experience the most significant change, with nearly 80% of the world’s population over 60 living in LMICs by 2050 [2]. This demographic shift is expected to transform societies across many spectrums, impacting healthcare systems, social welfare programs, economic productivity, and family structures [3].
As the older population continues to increase, there will be a corresponding rise in the demand for long-term care (LTC) services, encompassing home and community-based care, healthcare monitoring, rehabilitation, and therapy services. These services are defined as those that safeguard older persons’ intrinsic capacities and functional ability, ensuring they align with their fundamental rights, basic freedoms, and human dignity [4, 5]. As the healthcare system shifts away from being disease-based and evolves towards holistic and comprehensive care, the importance of LTC services in supporting older persons becomes increasingly acknowledged and emphasised [6]. In response, the World Health Organization (WHO) identified a need to promote health, prevent disease, maintain intrinsic capacity, and enable the functional ability of older persons by ensuring access to LTC [5]. The WHO has developed a public health framework for healthy ageing comprising three domains: health services, LTC, and environments [7]. These domains encompass various aspects of healthcare, such as preventing chronic conditions, facilitating early detection and control, reversing or mitigating declines in capacity, managing advanced chronic conditions, and promoting capacity-enhancing behaviours.
Evidence suggests that diminished functional ability in older persons correlates with increased utilisation of healthcare services, leading to higher treatment costs and a greater likelihood of institutionalisation [8,9,10]. Despite some progress in the formal delivery of LTC services in many LMICs, family members or caregivers continue to shoulder the bulk of LTC needs [6]. Thus, there exists a pressing need to integrate LTC into health systems delivery to ensure that services are readily accessible to support and prevent functional decline among older persons [11]. The WHO has developed guiding frameworks and models to facilitate the seamless integration of LTC into health system policies, promoting accessibility and efficacy in care delivery [12]. However, incorporating an effective LTC system is complex, often involving commitments across diverse care settings. In many LMICs, policymakers encounter the challenge of aligning LTC within broader health system perspectives, usually contending with limited resources and conflicting priorities [13, 14]. Therefore, it is crucial to identify, map, and summarise the global LTC interventions and services for older persons while considering their influence on healthcare utilisation.
While substantial evidence exists regarding the effectiveness of various LTC interventions [15,16,17,18], there are conflicting findings. To our knowledge, few studies have mapped the characteristics of LTC interventions [19, 20], but the impact of LTC interventions on healthcare utilisation is unknown. Owing to the abundance of knowledge on LTC interventions, we augmented and advanced the existing knowledge through a comprehensive scoping review focused on systematic reviews with meta-analyses. The primary objective is to examine and consolidate information on LTC interventions that influence healthcare utilisation among older persons. These findings are pivotal in guiding policy development, particularly in identifying and prioritising LTC services that positively contribute to the healthcare system and improve the overall care for older persons.
Methods
A scoping review was reported based on the methodological framework for scoping studies by Arksey and O’Malley [21] and Preferred Reporting Items for Systematic Review and Meta-analyses (PRISMA) guidelines [22]. The research protocol was registered as part of a more extensive study (Trial registration: NMRR-21-467-58076) and in the Open Science Framework (OSF) [23]. Due to the extent of the study scope and search, the study was amended from an umbrella review to a scoping review. While an umbrella review typically addresses a narrower research question, often focusing on specific interventions or outcomes [24], the current study encompasses a broader range of both interventions and outcomes. Therefore, it was determined that a scoping review would be a more appropriate methodology based on the research focus.
The scoping review specifically targeted systematic reviews accompanied by meta-analyses, delineated as articles explicitly identified as such in their title, abstract, or methods section. This allows the examination of a range of heterogeneous interventions that could be aggregated to assess and quantify their collective impact on healthcare utilisation. To provide a comprehensive overview of interventions considered in the meta-analysis, individual trials not pooled into meta-analyses in the articles were retained in this study.
Stage 1: identifying the research question
The scoping review aimed to address the following question: What insights does the existing systematic review with meta-analyses offer regarding the impact of LTC interventions on healthcare utilisation among older persons?
Stage 2: identifying relevant studies
A systematic search was performed on the following databases: PubMed, EBSCO CINAHL Plus, Cochrane Database Systematic Review, Embase, APA PsychINFO, EBM Reviews - Health Technology Assessment, and EBM Reviews - NHS Economic Evaluation Database. The search included Medical Subject Headings (MeSH) terms supplemented with a search of reference lists from identified studies (Additional file 1). The initial search occurred in November 2021, with three updated searches in June 2022, May 2023, and April 2024.
Stage 3: study selection
Inclusion criteria
Studies were eligible for inclusion if they were: a) Systematic reviews with meta-analyses encompassing Randomised Controlled Trials (RCTs) and observational studies investigating both single and multi-component LTC interventions or services; b) included older persons aged 60 years and above; c) targeted interventions or services in any setting, including home, community, healthcare facility, nursing homes or residential aged care facility; d) reported on health service utilisation as an outcome; and e) published between January 2010 and June 2022 in English. This study defined LTC as a wide range of interventions and services, such as managing chronic geriatric conditions, rehabilitation, palliation, promotion, and preventative services [25]. The search was limited to the year 2010 onwards to allow for the identification of recent evidence. As the aim of this study was to support health systems planning, only healthcare service utilisation reported from a health systems perspective was included, such as a) Hospital utilisation, b) Emergency department (ED) utilisation, c) Medication utilisation, and d) Primary care utilisation [26].
Exclusion criteria
Studies were excluded if: a) they included a disease-specific population; b) the target participants were not exclusively older persons and included a mixture of younger (below 60 years old) and older persons; c) reported outcomes focused exclusively on caregivers and/or health providers; d) reported on patient outcomes such as health-related quality of life; and e) focused exclusively on outcome measures for economic evaluation.
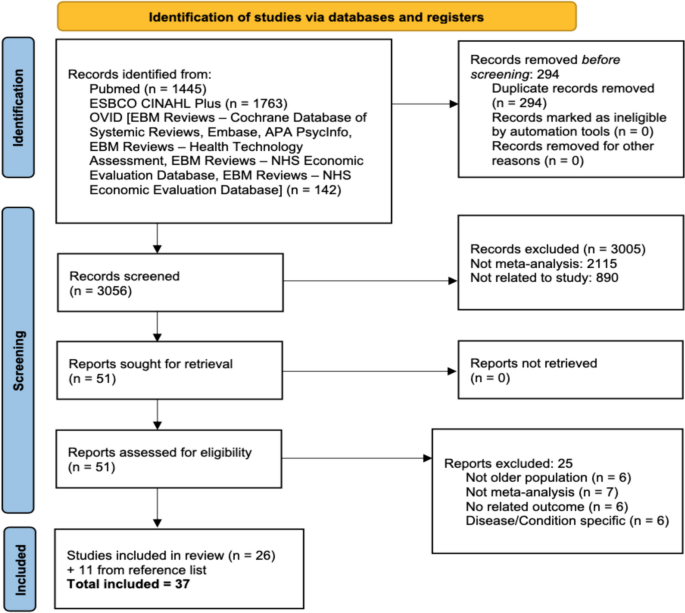
Screening and selection process
The selected studies were exported to a reference manager (EndNote X9) and deduplicated. Two reviewers independently screened the citation titles and abstracts for inclusion. The full text of the identified articles was retrieved and screened against the inclusion/exclusion criteria by another two independent reviewers. Any disagreements were resolved by consensus with a third reviewer.
Stage 4: charting the data
Two pairs of reviewers then independently extracted the included studies using a standardised, pre-piloted data extraction form. The extracted information included study demographics, information related to primary studies included in the review, and LTC interventions/services. Summary findings were recorded in Excel Microsoft Office 365 (Additional file 2).
Data synthesis and analysis
The results of the study were first described narratively. The LTC interventions were given a code based on the objective of the intervention in preventing or managing older persons’ intrinsic capacities or functional abilities. The coded LTC interventions were then mapped into several domains according to the WHO Healthy Ageing Framework [7], namely prevention activities, detection and control activities, management of chronic diseases, promotion and support of capacity-enhancing behaviours, ensuring a dignified late life, removing barriers to participation, and compensation for the loss of capacity by three independent reviewers. If needed, two other reviewers discussed any discrepancies and disagreements regarding the adjudication.
Interventions were then grouped into the four primary outcomes: hospital, emergency department, medication, and primary care utilisations and subdivided into separate domains. Hospital utilisation was further split into hospital admission, hospital readmission, length of stay or bed days. Emergency department (ED) utilisation was divided into ED visit, ED revisit, and length of stay. Medication utilisation refers to the number of drug use, and primary care utilisation refers to the number of visits.
Values extracted from all articles were reanalysed to standardise the findings, considering that various articles reported results in different units of measurement. Values were extracted across all interventions mentioned in the articles, irrespective of their inclusion in either meta-analyses or standalone analyses within the article. Trials from separate meta-analyses with similar intervention characteristics were analysed together unless the setting or follow-up duration differed. Redundant trials across different meta-analyses were removed, except in several situations whereby different values were extracted differently from the same trials. This discrepancy could arise from varying definitions of the outcomes among the authors or possibly from some authors reaching out to the primary author for supplementary data. The intervention durations were reclassified into four categories: less than six months, 7–12 months, 13–24 months, and 25–36 months for all outcomes. Consequently, the pooled interventions reported may deviate from the classification utilised in the original article. An illustration of the process flow is depicted in Additional File 3.
Due to the heterogeneity of included articles, RCTs and observational studies were analysed separately. Each association of long-term intervention with healthcare utilisations was reported in mean difference (MD) or odds ratio (OR) with a corresponding 95% confidence interval (CI) using the random-effects model, given the heterogeneity in design between and within studies [27]. The analysis was repeated using a fixed-effect model as a sensitivity analysis to investigate whether the method contributed to the observed high heterogeneity. When data from the articles were insufficient for reanalysis, we tried to contact the authors to gain the data. However, in cases where authors were not contactable, the data was extracted from the result as reported or marked as not reported (NR) when the data was unavailable. All statistical analyses were conducted with Stata version 14.0 (Stata Corp, College Station, TX, USA).
Assessment of methodological quality
Two independent reviewers assessed the methodological quality of the included studies using the A Measurement Tool to Assess Systematic Reviews-2 (AMSTAR-2) checklist [28]. The index rates the quality of the studies based on seven critical and nine non-critical domains. Studies were rated high, moderate, low, and critically low quality. To aid in interpreting results, we assessed the quality of evidence of each outcome using the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) [29]. The quality of evidence was evaluated based on five domains, including a) risk of bias in individual studies b), inconsistency c), indirectness d), imprecision, and e) publication bias, subsequently classified as high, moderate, low, or very low quality. The quality ratings assigned to the evidence indicate the level of assurance in the accuracy of the estimated effects [30].
Stage 5: collating, summarising, and reporting the results
All results were collated and summarised. The LTC interventions and their impacts on healthcare utilisation were presented.
Ethics considerations
This scoping review was part of a more extensive study, ‘Simulation of Long-Term Care for Elderly in Malaysia’ (MyLTC, Trial registration number: NMRR-21-467-58076). The MyLTC protocol was approved by the Medical Research and Ethics Committee (MREC), Ministry of Health Malaysia. The study was conducted by Good Clinical Practice guidelines and the Declaration of Helsinki.
Results
The initial search identified 3,350 records, with 3,056 records screened after deduplication. Fifty-one full-text articles were screened, and 26 articles were selected after exclusion. An additional 11 studies were sourced from the reference list search. A total of 37 articles were included in this review (Fig. 1). The reasons for exclusion are provided in Additional File 4.
Characteristics and methodological quality of articles exploring associations of long-term care interventions with healthcare utilisations for older persons
Of the 37 articles included, 17 were RCTs or cluster RCTs, while the remaining were mixed study designs. The median and interquartile range (IQR) for the number of studies per article was 17 [12,13,14,15,16,17,18,19,20,21,22,23,24]. The sample sizes ranged from 811 to the largest, involving 108,838 participants, with a median (IQR) of 9,679 (3,976 − 18,992). The duration of follow-up varies between studies, with the shortest follow-up within one week and the longest over 60 months. A total of 82 outcomes across all articles were identified. The most studied outcomes reported were hospital readmission (n = 19, 23.2%) and hospital admission (n = 18, 21.9%).
Most articles were rated either low or critically low in the methodological assessment using AMSTAR-2 (Table 1 and Additional file 5). This was mainly due to methodological issues, including the need for more justification for excluding individual studies and a lack of assessment regarding publication bias and its potential impact. The descriptive characteristics of the 37 eligible articles are provided in Table 1.
Characteristics and mapping of long-term care interventions to the healthy ageing Framework
Altogether, 37 LTC interventions were included in the analysis (Table 2). Although various interventions share similar names, they were implemented in distinct settings, yielded diverse outcomes, featured varying durations of outcomes follow-up, or engaged different providers, warranting separate descriptions. No overlap of intervention from the same meta-analyses was identified.
Most interventions involved multidisciplinary teams or coordination, with only six interventions among a single healthcare professional [37, 42, 45, 50, 52, 67]. The most common settings were community-based or involved transfer back to the community following discharge from the hospital, including the older person’s home, with 17 interventions. Nine interventions were set in long-term care institutions [31, 44, 45, 51, 52, 55, 58, 64, 65], with the remaining in hospitals or in mixed settings. The most common type of intervention was the Comprehensive Geriatric Assessment (CGA) (n = 8, 23.5%). However, the intervention was applied across various settings, delivered by different teams of healthcare professionals, and had different follow-up durations. Mapping to the WHO Healthy Ageing Framework revealed that 11 interventions focused on managing chronic conditions [31, 42, 44, 45, 49, 52, 53, 55, 58, 64, 67], ten supported capacity enhancement [37, 41, 46, 51, 56, 59, 62, 63, 65, 66], eight were on early detection and control [33, 35, 36, 38,39,40, 43, 60], six were to promote capacity enhancement [32, 47, 48, 50, 57, 61], and one each for prevention of chronic conditions [54] and compensation of capacity [34].
Associations between long-term care interventions with healthcare utilisations among older persons
One hundred and twelve associations were reported between LTC interventions and healthcare utilisations, mostly on hospital utilisation (n = 86, 76.8%). Seventeen associations were reported on ED utilisation, six on medication utilisation and three on primary care service utilisation (Additional file 6). Twenty-two out of the 112 associations (19.6%) were statistically significant (Table 3). The GRADE reporting for all associations is reported in Additional File 7.
Hospital utilisation
Altogether, 35 associations discussed hospital admission (Additional file 6). Six associations (17.1%) reflected a significant reduction in the risk of hospital admission among older persons. The associations mapped to five interventions: Deprescribing interventions [64], community-based aged care [47], preventive home visits [48], CGA implemented in a community setting [33], and medication review by pharmacists in Long-term Care Facility (LTCF) [52]. Three of the five significant interventions were implemented in the community-based setting (community-based aged care [47], preventive home visits [48], and CGA implemented in a community setting [33]). Among these five interventions, only preventive home visits at 7–12 months follow-up (OR: 0.73, 95% CI: 0.59, 0.91, p = 0.005) received a moderate GRADE quality of evidence rating [48], with all other interventions rated either low or very low quality.
For hospital readmission, there were 32 associations (Additional file 6). Eight associations (25%) from six interventions were significantly associated with hospital readmission. All six interventions involved implementation in a community setting or a transfer back into the community following discharge from the hospital [41, 47, 51, 56, 63, 65]. Six associations were found to reduce hospital readmission, with only one intervention, caregiver integration during discharge planning at 1–6 months follow-up (OR: 0.68, 95% CI: 0.57, 0.81, p < 0.001), had high-quality evidence [51]. This intervention included 13 studies with a low heterogeneity. Another intervention found to have a moderate quality of evidence in reducing hospital readmission was continuity of care at a 7–12 months follow-up (OR: 0.76, 95% CI: 0.61, 0.95, p = 0.018) [41]. The other two interventions representing four associations with low and very low-quality evidence were integrating primary healthcare in aftercare [63] and transitional care programs for community-dwelling older persons [56]. The remaining two interventions increased the odds or risk of hospital readmissions among older persons (transitional care programs for long-term care facility residents [65] and community-based aged-care interventions [47]). However, both interventions received low and very low-quality evidence.
There were 17 associations regarding the outcome of length of stay (Additional file 6). Three associations (17.6%) from three interventions demonstrated significant reductions in the length of hospital stay [43, 54, 59]. All interventions were implemented in a hospital setting. Perioperative geriatric interventions at a 12-month follow-up, which involved twelve studies, were the only intervention with a moderate quality of evidence (MD: -1.50, 95% CI: -2.24, -0.76, p < 0.001) and low heterogeneity (32.7%) [54]. The remaining two interventions, early support discharge [59] and CGA, were implemented in the ward and had low or very low-quality evidence and high or moderate heterogeneity.
Utilisation of emergency department
ED utilisation was found to have 17 associations (Additional file 6). Three associations (17.6%) from three interventions significantly reduced ED utilisation. Two were on ED visits (community-based case management [49] and CGA implemented in a community setting [33]), and one was on the length of ED stay (transitional care programs for long-term care facility residents [65]). However, all three interventions were found to have either low or very low-quality evidence.
Utilisation of medications and prescriptions
The outcome of drug use had six associations (Additional file 6). Only one association (16.7%) from an intervention, anti-microbial stewardship at a 12-month follow-up, significantly reduced the number of drugs used among older persons (MD: -0.47, 95% CI: -0.87, -0.07, p = 0.02) [58]. However, this association was graded as having very low quality and high heterogeneity.
Utilisation of primary care
Three associations were found for the outcome of primary care visits (Additional file 6). One association (33.3%) from an intervention was statistically significant. A community-based aged care intervention increased the number of visits (RR: 1.43, 95% CI: 1.11, 1.18, p: 0.002) [47]. The quality of evidence was found to be very low.
Sensitivity analysis
The re-analysis of associations with high heterogeneity using a fixed-effect model did not significantly alter the associations between the intervention and the outcome measured.
Discussion
Thirty-seven meta-analyses were included in the study, comprising 112 associations between various LTC interventions and healthcare utilisations. Four of the 22 statistically significant associations were supported by suggestive or convincing evidence and remarked as either high or moderate quality of evidence. These associations include four different LTC interventions: preventive home visits were found to reduce hospital admission [48], caregiver integration during discharge planning [51], and continuity of care [41], reduced hospital readmission, and perioperative geriatric interventions [54] reduced the length of hospital stay. There was no convincing evidence on the association between LTC and ED, medication and primary care utilisation.
Mapping the LTC interventions to the WHO Healthy Ageing Framework revealed that the most extensive domain explored was managing chronic conditions (11 out of 37 interventions), followed by support of capacity enhancement (9 out of 37 interventions). These findings fit well with the aims of the healthy ageing framework, whereby both domains were crucial in preventing substantial loss of capacity among older persons [7]. However, it represents opportunities or a need to explore services in other domains, facilitating the evidence-based implementation of more comprehensive LTC services. This is essential for supporting health systems in meeting the evolving needs of the ageing population, ensuring that older persons receive high-quality and coordinated care for their well-being. Most interventions were found to be implemented in a community setting or involved a transfer back into the community following discharge from the hospital. This finding aligns with other evidence emphasising that while LTC services can be implemented in various settings, a community-based approach offers the most benefit to older persons [7, 19, 68]. However, this finding could also be due to the exclusion of interventions among disease-specific conditions, which may have been more extensively implemented in hospital or institutional-based settings. Therefore, future comparisons and discussions should consider the contextual factors of LTC implementations, including the specific settings in which they occur.
Most interventions involved multidisciplinary teams of various health, social care, and community-based providers, supporting findings and recommendations elsewhere [7, 20]. Indeed, the involvement of relevant providers in caring for and providing LTC services for older persons is essential in ensuring that all their needs are adequately assessed and addressed in an integrated and coordinated approach [12, 68]. CGA emerged as the most common intervention recurring across all meta-analyses. It signifies the importance of a thorough clinical and psychological evaluation and the presence of support evaluation in delivering care to older persons [69]. However, since this review identified interventions labelled as ‘long-term care’, it could also suggest that CGA was among the most developed LTC interventions that have been assessed and evaluated across multitudes of different outcomes, including healthcare utilisations, which highlights future research opportunities for evaluating other LTC interventions that were less explored.
This review found suggestive evidence that preventive home visits [48] reduced the likelihood of hospital admission among older persons. The service was provided by a multidisciplinary team offering comprehensive care, including assessment of health and support needs, referral to relevant care providers, medication review, and rehabilitation at the older person’s home [48]. The approach ensures early detection of diseases and conditions, improves access to care, and offers a large spectrum of services that are otherwise not provided during routine care [70]. The finding reciprocates a recent umbrella review reporting that home visits were favourable in reducing hospital admission frequency [71]. As debated in the review, the definitions and components of what constituted ‘home visits’ vary across studies and warrant further evaluation. Nevertheless, the heterogeneity for this intervention was found to be low in this study [72].
Caregiver integration during discharge planning had convincing evidence in reducing hospital readmission [51]. The service included linking caregivers to external or community resources, preparing written care plans, performing caregiver assessment, medication reconciliation, and iterative teaching sessions in providing care, all planned and executed during the discharge process of older persons from the hospital. Discharge planning implies a comprehensive plan was prepared based on the anticipated healthcare needs of the older persons [73]. Including caregivers in the discharge planning enhanced the care by delegating part of the responsibilities to the person managing the patient [74]. Similarly, continuity of care upon discharge from the hospital was found to have suggestive evidence in reducing hospital readmission [41]. Early hospital readmissions are often due to insufficient recognition of a patient’s needs, leading to unaddressed issues and poor management at home [75]. Ensuring that care is continued primarily through care coordination between hospital and primary healthcare providers means the underlying disease that caused the earlier hospital admission is appropriately managed. A recurrent episode requiring further hospitalisation (readmission) is thus prevented [41]. The overarching idea was that to reduce hospital readmission, there was a need for a comprehensive assessment and identification of an older person’s health and other requirements within the hospital setting before discharge. This process involves crafting a detailed, coordinated care plan that includes caregivers and other healthcare providers, ensuring a smooth transition and effective ongoing care management post-discharge.
Perioperative geriatric interventions, defined as any program aiming to enhance clinical outcomes of older persons having surgeries performed, was the only intervention with suggestive evidence of reducing the length of stay in hospital [54]. The interventions mitigate the increased risk associated with surgeries by customising care to the specific needs of the patients, potentially preventing functional decline and related complications [54]. No convincing LTC intervention was found to influence ED, drug use, and primary care utilisation. This could be due to the limited number of studies that evaluated these outcomes, warranting future research.
Implications for practice and future research
This scoping review offers an extensive summary across meta-analyses on existing LTC interventions that impacted healthcare utilisations. Since the scope of this study covers the general older population, the findings may be beneficial for policymakers looking to implement LTC interventions at a macro rather than disease-specific level. The review found a few effective LTC interventions in reducing healthcare utilisations. Nevertheless, from the health systems point of view, it provides insights for potential interventions that could alleviate the strain on healthcare systems, exacerbated by the increasing prevalence of non-communicable diseases (NCDs) and age-related functional disabilities [76]. It also means future research may be directed towards exploring the impact of more and newer LTC interventions towards healthcare utilisations. The limited number of existing studies assessing the impact of LTC interventions on healthcare utilisation may partly explain the little evidence found through this study. Still, it also suggests that LTC interventions could have broader positive effects on various other outcomes, including individual well-being, mortality, clinical outcomes, and functional limitations, which were not within the scope of the current study. Despite the small number of effective LTC interventions found, the overall picture suggests that LTC interventions need to move away from hospital or institution-based implementations to the community or older persons’ homes. Such a move offers integrated, person-centred care at the place most comfortable for the older person, increasing adherence to care [77]. Comprehensive assessment identifying all aspects of the needs of older persons while being hospitalised, coupled with a properly documented detailed discharge plan, which includes roles of carers and other professionals that will continue the care upon discharge, is crucial in ensuring older persons’ well-being, hence impacting the subsequent healthcare utilisation.
Limitations
This scoping review has several limitations. The search strategy relied on interventions labelled ‘long-term care’ or other terms referring to LTC interventions. While the keywords postulated in the study covered as comprehensive LTC interventions as possible, more interventions may have served LTC functions but were not labelled as such. While the study covers multiple outcomes related to healthcare utilisations, more outcomes existed that were not included in the current review. For example, preventable hospitalisation, preventable ED visits, and time to hospitalisation were among various related outcomes not included in the present review. While the inclusion of meta-analysis in our review offers a comprehensive overview of the outcomes’ direction and strength across different interventions, it is essential to acknowledge the diversity in implementation, contextual backgrounds, and settings of various other interventions, making it impossible for studies to pool and analyse all existing interventions. As a result, while our current review encompasses broad LTC interventions for older persons analysed within a systematic review with meta-analysis, it is essential to recognise that a wealth of additional evidence available could offer further insights into practical strategies for reducing healthcare utilisation among this population. The review also did not directly assess the quality of individual primary studies included in each meta-analysis but instead relied on the assessment reported by the authors. A further limitation was that we did not perform subgroup analysis (for example, by age groups, sex, and location where the intervention was delivered) due to the lack of data for grading the quality evidence for most interventions.
Conclusion
The findings of this study suggest LTC interventions could benefit from transitioning to a community-based setting, involving a multidisciplinary team including the carers that offer a large spectrum of services fulfilling various needs of older persons, incorporate comprehensive and holistic assessment plan, and include a detailed discharge plan that ensures integrated, coordinated and continuous care is achieved. However, the current evidence pertains to hospital utilisation, with more research needed to identify interventions impacting other healthcare utilisations. Nevertheless, the present findings offer insights into effective LTC interventions that may be considered for implementation by policymakers at a macro level.
Availability of data and materials
The data analysed for this review is part of the ‘Simulation of Long-Term Care for Elderly in Malaysia’ (MyLTC) study and belongs to the Ministry of Health Malaysia. Requests for the data can be obtained from the Principal Investigator, Dr Fun Weng Hong, through email: fun.wh@moh.gov.my with permission from the Director-General of Health, Malaysia.
Abbreviations
- AMSTAR-2:
-
A Measurement Tool to Assess Systematic Reviews-2
- CGA:
-
Comprehensive Geriatric Assessment
- CI:
-
Confidence interval
- ED:
-
Emergency department
- GRADE:
-
Grading of Recommendations, Assessment, Development, and Evaluations
- IQR:
-
Interquartile range
- LMICs:
-
Low- and middle-income countries
- LTC:
-
Long-term care
- LTCF:
-
Long-term Care Facility
- MD:
-
Mean difference
- MeSH:
-
Medical Subject Headings
- MREC:
-
Medical Research and Ethics Committee
- NCDs:
-
Non-communicable diseases
- NR:
-
Not reported
- OR:
-
Odds ratio
- OSF:
-
Open Science Framework
- PRISMA:
-
Preferred Reporting Items for Systematic Review and Meta-analyses
- RCTs:
-
Randomised Controlled Trials
- RR:
-
Risk ratio
- WHO:
-
World Health Organization
References
United Nations Department of Economic and Social Affairs, Population Division. World Population Prospects 2022: Summary of Results. New York; 2022.
World Health Organization. Ageing and health 2022 [ https://www.who.int/news-room/fact-sheets/detail/ageing-and-health.
European Commission. European Commission Report on the Impact of Demographic Change. 2020.
Kane RA, Kane RL, Ladd RC. The heart of long term care. USA: Oxford University Press; 1998.
World Health Organization. Decade of healthy ageing: baseline report. 2021.
World Health Organization. Long-term care financing: lessons for low-and middle-income settings: brief 1: drivers of the demand for long-term care. 2024.
Beard JR, Officer A, De Carvalho IA, Sadana R, Pot AM, Michel J-P, et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387(10033):2145–54.
Fried TR, Bradley EH, Williams CS, Tinetti ME. Functional disability and health care expenditures for older persons. Arch Intern Med. 2001;161(21):2602–7.
Miller EA, Weissert WG. Predicting elderly people’s risk for nursing home placement, hospitalization, functional impairment, and mortality: a synthesis. Med care Res Rev. 2000;57(3):259–97.
Palladino R, Tayu Lee J, Ashworth M, Triassi M, Millett C. Associations between multimorbidity, healthcare utilisation and health status: evidence from 16 European countries. Age Ageing. 2016;45(3):431–5.
Tessier L, de Wulf N, Momose Y. Long-term care in the context of population ageing: A rights-based approach to universal coverage: ILO Working Paper. Geneva: International Labour Office; 2022.
Brodsky J, Habib J, Hirschfeld M. Key policy issues in long-term care. Geneva: World Health Organization; 2003.
Feng Z. Global convergence: aging and long-term care policy challenges in the developing world. J Aging Soc Policy. 2019;31(4):291–7.
World Health Organization. Long-term care financing: lessons for low-and middle-income settings: brief 2: decisions about population coverage of long-term care. 2024.
Abbott RA, Whear R, Thompson-Coon J, Ukoumunne OC, Rogers M, Bethel A, et al. Effectiveness of mealtime interventions on nutritional outcomes for the elderly living in residential care: a systematic review and meta-analysis. Ageing Res Rev. 2013;12(4):967–81.
Cao Py Z, Qh X, Mz K, Ln XL. The effectiveness of exercise for fall prevention in nursing home residents: a systematic review meta-analysis. J Adv Nurs. 2018;74(11):2511–22.
Frost R, Belk C, Jovicic A, Ricciardi F, Kharicha K, Gardner B, et al. Health promotion interventions for community-dwelling older people with mild or pre-frailty: a systematic review and meta-analysis. BMC Geriatr. 2017;17:1–13.
Giné-Garriga M, Roqué-Fíguls M, Coll-Planas L, Sitjà-Rabert M, Salvà A. Physical exercise interventions for improving performance-based measures of physical function in community-dwelling, frail older adults: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2014;95(4):753–69. e3.
Arias-Casais N, Thiyagarajan JA, Perracini MR, Park E, Van den Block L, Sumi Y, et al. What long-term care interventions have been published between 2010 and 2020? Results of a WHO scoping review identifying long-term care interventions for older people around the world. BMJ Open. 2022;12(1):e054492.
Bayly J, Bone AE, Ellis-Smith C, Yaqub S, Yi D, Nkhoma KB, et al. Common elements of service delivery models that optimise quality of life and health service use among older people with advanced progressive conditions: a tertiary systematic review. BMJ Open. 2021;11(12):e048417.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Reviews. 2015;4(1):1–9.
Balqis-Ali NZ, Jawahir S, Mohd Shaffie SS, Azlan UW, Fun WH, Chan YM, Lim AWY, Lee SWH. The impact of long-term care interventions on healthcare utilisation among older persons: A scoping review of meta-analyses [Internet]. OSF; 2024. [Available from: https://www.osf.io/sjfzn].
Aromataris E, Fernandez RS, Godfrey C, Holly C, Khalil H, Tungpunkom P. Methodology for JBI umbrella reviews. Joanna Briggs Institute Reviewers’ Manual. Australia: The Joanna Briggs Institute; 2014.
World Health Organization. Rebuilding for sustainability and resilience: strengthening the integrated delivery of long-term care in the European Region. Copenhagen: World Health Organization, Regional Office for Europe; 2022.
Arueira Chaves L, de Serio S, dos Santos D, Rodrigues Campos M, Luiza VL. Use of health outcome and health service utilization indicators as an outcome of access to medicines in Brazil: perspectives from a literature review. Public Health Rev. 2019;40(1):1–20.
Dettori JR, Norvell DC, Chapman JR. Fixed-effect vs random-effects models for meta-analysis: 3 points to consider. Global Spine J. 2022;12(7):1624–6.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008–4008.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–6.
Almutairi H, Stafford A, Etherton-Beer C, Flicker L. Optimisation of medications used in residential aged care facilities: a systematic review and meta-analysis of randomised controlled trials. BMC Geriatr. 2020;20(1):1–19.
Beswick AD, Gooberman-Hill R, Smith A, Wylde V, Ebrahim S. Maintaining independence in older people. Reviews Clin Gerontol. 2010;20(2):128–53.
Briggs R, McDonough A, Ellis G, Bennett K, O'Neill D, Robinson D. Comprehensive Geriatric Assessment for community‐dwelling, high‐risk, frail, older people. Cochrane Database Syst Reviews. 2022;5(5):CD012705.
Cochrane A, Furlong M, McGilloway S, Molloy DW, Stevenson M, Donnelly M. Time‐limited home‐care reablement services for maintaining and improving the functional independence of older adults. Cochrane Database Syst Rev. 2016;10(10):CD010825.
Conroy SP, Stevens T, Parker SG, Gladman JR. A systematic review of comprehensive geriatric assessment to improve outcomes for frail older people being rapidly discharged from acute hospital:‘interface geriatrics’. Age Ageing. 2011;40(4):436–43.
Deschodt M, Flamaing J, Haentjens P, Boonen S, Milisen K. Impact of geriatric consultation teams on clinical outcome in acute hospitals: a systematic review and meta-analysis. BMC Med. 2013;11:1–13.
Deschodt M, Laurent G, Cornelissen L, Yip O, Zuniga F, Denhaerynck K, et al. Core components and impact of nurse-led integrated care models for home-dwelling older people: a systematic review and meta-analysis. Int J Nurs Stud. 2020;105:103552.
Ekdahl A, Sjöstrand F, Ehrenberg A, Oredsson S, Stavenow L, Wisten A, et al. Frailty and comprehensive geriatric assessment organized as CGA-ward or CGA-consult for older adult patients in the acute care setting: a systematic review and meta-analysis. Eur Geriatr Med. 2015;6(6):523–40.
Ellis G, Gardner M, Tsiachristas A, Langhorne P, Burke O, Harwood RH, et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev. 2017;9(9):CD006211.
Ellis G, Whitehead MA, Robinson D, O’Neill D, Langhorne P. Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ. 2011;343:d6553.
Facchinetti G, D’Angelo D, Piredda M, Petitti T, Matarese M, Oliveti A, et al. Continuity of care interventions for preventing hospital readmission of older people with chronic diseases: a meta-analysis. Int J Nurs Stud. 2020;101:103396.
Forster A, Young J, Lambley R, Langhorne P. Medical day hospital care for the elderly versus alternative forms of care. Cochrane Database Syst Rev. 2008;(4):CD001730.
Fox MT, Persaud M, Maimets I, O’Brien K, Brooks D, Tregunno D, et al. Effectiveness of acute geriatric unit care using acute care for elders components: a systematic review and meta-analysis. J Am Geriatr Soc. 2012;60(12):2237–45.
Hill-Taylor B, Walsh K, Stewart S, Hayden J, Byrne S, Sketris IS. Effectiveness of the STOPP/START (Screening Tool of older persons’ potentially inappropriate Prescriptions/Screening tool to alert doctors to the right treatment) criteria: systematic review and meta‐analysis of randomized controlled studies. J Clin Pharm Ther. 2016;41(2):158–69.
Lee JK, Slack MK, Martin J, Ehrman C, Chisholm-Burns M. Geriatric patient care by US pharmacists in healthcare teams: systematic review and meta‐analyses. J Am Geriatr Soc. 2013;61(7):1119–27.
Lowthian JA, McGinnes RA, Brand CA, Barker AL, Cameron PA. Discharging older patients from the emergency department effectively: a systematic review and meta-analysis. Age Ageing. 2015;44(5):761–70.
Luker JA, Worley A, Stanley M, Uy J, Watt AM, Hillier SL. The evidence for services to avoid or delay residential aged care admission: a systematic review. BMC Geriatr. 2019;19:1–20.
Mayo-Wilson E, Grant S, Burton J, Parsons A, Underhill K, Montgomery P. Preventive home visits for mortality, morbidity, and institutionalization in older adults: a systematic review and meta-analysis. PLoS ONE. 2014;9(3):e89257.
Poupard N, Tang CY, Shields N. Community-based case management does not reduce hospital admissions for older people: a systematic review and meta-analysis. Aust Health Rev. 2019;44(1):83–92.
Spiers G, Matthews F, Moffatt S, Barker R, Jarvis H, Stow D, et al. Impact of social care supply on healthcare utilisation by older adults: a systematic review and meta-analysis. Age Ageing. 2019;48(1):57–66.
Rodakowski J, Rocco PB, Ortiz M, Folb B, Schulz R, Morton SC, et al. Caregiver integration during discharge planning for older adults to reduce resource use: a metaanalysis. J Am Geriatr Soc. 2017;65(8):1748–55.
Sadowski CA, Charrois TL, Sehn E, Chatterley T, Kim S. The role and impact of the pharmacist in long-term care settings: a systematic review. J Am Pharmacists Association. 2020;60(3):516–24 e2.
Tecklenborg S, Byrne C, Cahir C, Brown L, Bennett K. Interventions to reduce adverse drug event-related outcomes in older adults: a systematic review and meta-analysis. Drugs Aging. 2020;37:91–8.
Thillainadesan J, Yumol MF, Hilmer S, Aitken SJ, Naganathan V. Interventions to improve clinical outcomes in older adults admitted to a surgical service: a systematic review and meta-analysis. J Am Med Dir Assoc. 2020;21(12):1833–43. e20.
Wallerstedt SM, Kindblom JM, Nylén K, Samuelsson O, Strandell A. Medication reviews for nursing home residents to reduce mortality and hospitalization: systematic review and meta-analysis. Br J Clin Pharmacol. 2014;78(3):488–97.
Weeks LE, Macdonald M, Martin-Misener R, Helwig M, Bishop A, Iduye DF, et al. The impact of transitional care programs on health services utilization in community-dwelling older adults: a systematic review. JBI Evid Synthesis. 2018;16(2):345–84.
Wong KC, Wong FKY, Yeung WF, Chang K. The effect of complex interventions on supporting self-care among community-dwelling older adults: a systematic review and meta-analysis. Age Ageing. 2018;47(2):185–93.
Crespo-Rivas JC, Guisado-Gil AB, Peñalva G, Rodríguez-Villodres Á, Martín-Gandul C, Pachón-Ibáñez ME, et al. Are antimicrobial stewardship interventions effective and safe in long-term care facilities? A systematic review and meta-analysis. Clin Microbiol Infect. 2021;27(10):1431–8.
Williams S, Morrissey A-M, Steed F, Leahy A, Shanahan E, Peters C, et al. Early supported discharge for older adults admitted to hospital with medical complaints: a systematic review and meta-analysis. BMC Geriatr. 2022;22(1):302.
O’Shaughnessy Í, Robinson K, O’Connor M, Conneely M, Ryan D, Steed F, et al. Effectiveness of acute geriatric unit care on functional decline, clinical and process outcomes among hospitalised older adults with acute medical complaints: a systematic review and meta-analysis. Age Ageing. 2022;51(4):afac081.
Lin I, Glinsky J, Dean C, Graham P, Scrivener K. Effectiveness of home-based exercise for improving physical activity, quality of life and function in older adults after hospitalisation: a systematic review and meta-analysis. Clin Rehabil. 2022;36(9):1170–85.
Van Grootven B, Flamaing J, Dierckx de Casterlé B, Dubois C, Fagard K, Herregods MC, et al. Effectiveness of in-hospital geriatric co-management: a systematic review and meta-analysis. Age Ageing. 2017;46(6):903–10.
Li R, Geng J, Liu J, Wang G, Hesketh T. Effectiveness of integrating primary healthcare in aftercare for older patients after discharge from tertiary hospitals—a systematic review and meta-analysis. Age Ageing. 2022;51(6):afac151.
Kua C-H, Mak VS, Lee SWH. Health outcomes of deprescribing interventions among older residents in nursing homes: a systematic review and meta-analysis. J Am Med Dir Assoc. 2019;20(3):362–72. e11.
Birtwell K, Planner C, Hodkinson A, Hall A, Giles S, Campbell S, et al. Transitional care interventions for older residents of long-term care facilities: a systematic review and meta-analysis. JAMA Netw Open. 2022;5(5):e2210192–e.
Tomlinson J, Cheong V-L, Fylan B, Silcock J, Smith H, Karban K, et al. Successful care transitions for older people: a systematic review and meta-analysis of the effects of interventions that support medication continuity. Age Ageing. 2020;49(4):558–69.
Lee SWH, Mak VSL, Tang YW. Pharmacist services in nursing homes: a systematic review and meta-analysis. Br J Clin Pharmacol. 2019;85(12):2668–88.
Tamiya N, Noguchi H, Nishi A, Reich MR, Ikegami N, Hashimoto H, et al. Population ageing and wellbeing: lessons from Japan’s long-term care insurance policy. Lancet. 2011;378(9797):1183–92.
Parker SG, McCue P, Phelps K, McCleod A, Arora S, Nockels K, et al. What is comprehensive geriatric assessment (CGA)? An umbrella review. Age Ageing. 2018;47(1):149–55.
Rosenberg T. Acute hospital use, nursing home placement, and mortality in a frail community-dwelling cohort managed with Primary Integrated Interdisciplinary Elder Care at Home. J Am Geriatr Soc. 2012;60(7):1340–6.
Eltaybani S, Kawase K, Kato R, Inagaki A, Li C-C, Shinohara M, et al. Effectiveness of home visit nursing on improving mortality, hospitalization, institutionalization, satisfaction, and quality of life among older people: umbrella review. Geriatr Nurs. 2023;51:330–45.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Craven E, Conroy S. Hospital readmissions in frail older people. Reviews Clin Gerontol. 2015;25(2):107–16.
Family Caregiver Alliance. Caregiver assessment: principles, guidelines and strategies for change: report from a National Consensus Development Conference. San Francisco; 2006.
Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med. 2016;374(16):1543–51.
Holmes W. Projecting the need for and cost of long-term care for older persons. 2021.
Sanerma P, Miettinen S, Paavilainen E, Åstedt-Kurki P. A client-centered approach in home care for older persons–an integrative review. Scand J Prim Health Care. 2020;38(4):369–80.
Acknowledgements
We thank the Director-General of Health, Ministry of Health Malaysia, for permission to publish this review.
Funding
This review was part of a more extensive study, ‘Simulation of Long-Term Care for Elderly in Malaysia (MyLTC)’ (Trial registration: NMRR-21-467-58076). The MyLTC study is funded by the Ministry of Health Malaysia (NIH/800-3/2/1 Jilid 8 (35), Warrant number: 91000050). Part of the funding was used to support the conduct of this review.
Author information
Authors and Affiliations
Contributions
NZB, YMC, SJ, and AL contributed to the early conception and study design. NZB, YMC, SJ, AL, WHF, and SWHL conceived and designed the review. NZB, YMC, SJ, AL, UWA, and SMS performed the review. SWHL provided technical advice on data extraction and analysis. NZB, YMC, SJ, AL, UWA, SMS and WHF analysed and interpreted the data. NZB, YMC, SJ, AL, UWA, SMS, WHF, and SWHL contributed to the writing and reviewing of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This scoping review was part of a more extensive study, ‘Simulation of Long-Term Care for Elderly in Malaysia’ (MyLTC, Trial registration number: NMRR-21-467-58076). The MyLTC protocol was approved by the Medical Research and Ethics Committee (MREC), Ministry of Health Malaysia. The study was conducted by Good Clinical Practice guidelines and the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12877_2024_5097_MOESM6_ESM.docx
Additional file 6. Summary of associations between long-term care interventions with hospital utilisation among older persons
12877_2024_5097_MOESM9_ESM.docx
Additional file 9. Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Balqis-Ali, N.Z., Jawahir, S., Chan, Y.M. et al. The impact of long-term care interventions on healthcare utilisation among older persons: a scoping review of reviews. BMC Geriatr 24, 484 (2024). https://doi.org/10.1186/s12877-024-05097-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05097-9