- Research
- Open access
- Published:
Impact of frailty on the outcomes of patients undergoing degenerative spine surgery: a systematic review and meta-analysis
BMC Geriatrics volume 23, Article number: 771 (2023)
Abstract
Background
Degenerative spinal diseases are common in older adults with concurrent frailty. Preoperative frailty is a strong predictor of adverse clinical outcomes after surgery. This study aimed to investigate the association between health-related outcomes and frailty in patients undergoing spine surgery for degenerative spine diseases.
Methods
A systematic review and meta-analysis were performed by electronically searching Ovid-MEDLINE, Ovid-Embase, Cochrane Library, and CINAHL for eligible studies until July 16, 2022. We reviewed all studies, excluding spinal tumours, non-surgical procedures, and experimental studies that examined the association between preoperative frailty and related outcomes after spine surgery. A total of 1,075 articles were identified in the initial search and were reviewed by two reviewers, independently. Data were subjected to qualitative and quantitative syntheses by meta-analytic methods.
Results
Thirty-eight articles on 474,651 patients who underwent degenerative spine surgeries were included and 17 papers were quantitatively synthesized. The health-related outcomes were divided into clinical outcomes and patient-reported outcomes; clinical outcomes were further divided into postoperative complications and supportive management procedures. Compared to the non-frail group, the frail group was significantly associated with a greater risk of high mortality, major complications, acute renal failure, myocardial infarction, non-home discharge, reintubation, and longer length of hospital stay. Regarding patient-reported outcomes, changes in scores between the preoperative and postoperative Oswestry Disability Index scores were not associated with preoperative frailty.
Conclusions
In degenerative spinal diseases, frailty is a strong predictor of adverse clinical outcomes after spine surgery. The relationship between preoperative frailty and patient-reported outcomes is still inconclusive. Further research is needed to consolidate the evidence from patient-reported outcomes.
Background
As the incidence of degenerative spinal diseases has increased and with advancements in medical technology [1, 2], the number of older adults undergoing spine surgeries has increased [3, 4]. Accordingly, difficulties encountered during spine surgeries have also increased [4, 5]. Because the outcomes of patients undergoing spine surgery are affected by their preoperative characteristics [6,7,8], it becomes imperative to gain insights into factors that may impact postoperative outcomes in this population, including frailty. Frailty is defined as a multidimensional state of loss of physical, cognitive, social, and psychological functioning [9]. The older the age, the higher the frailty; however, compared to chronological age, frailty status can better predict complications and mortality following spine surgery [10]. Most patients undergoing spine surgeries are prefrail or frail [7, 11], conditions which are often associated with preoperative pain, spinal deformity, and reduced ability to perform activities of daily living. For spine surgery, the incidence of postoperative complications and non-home discharge, length of hospital stay, and mortality rates are higher among patients with preoperative frailty than among those without [7, 12]. Therefore, preoperative risk stratification of frailty is helpful for predicting postoperative deterioration; this in turn can help prevent the worsening of outcomes after a spine surgery [9].
Patients with frailty who have undergone spine surgery do not experience the same level of benefit in terms of clinical outcomes (COs) as those who are not frail [13, 14]. Even then, such patients often opt for spine surgery to alleviate pain and improve function rather than for survival (unlike patients who opt for cancer surgery) [15]. Therefore, providing patients with information on the benefits of patient-reported outcomes (PROs) after spine surgery can help them make informed decisions and receive more patient-centred care. With the increased emphasis on the importance of PROs, research has increasingly focused on how PROs in frail patients have changed following spine surgery [13, 16]. However, there is a lack of understanding of the benefits and expected types of PROs in spine surgery. Therefore, a systematic literature review and meta-analysis of the relationship between preoperative frailty and the postoperative outcomes of surgery for patients with degenerative spinal disease is necessary.
A 2021 systematic review and meta-analysis of 32 studies on preoperative frailty and outcomes of spine surgery revealed that frailty was associated with increased adverse events, mortality, length of hospital stay, readmission, reoperation, non-home discharge, intensive care unit stay, and PROs following a spine surgery [17]. However, this review had the following limitations: studies on simple procedures such as kyphoplasty were included in the review; therefore, the risk of bias regarding non-surgical procedures could not be ruled out. Furthermore, because disease pathogenesis and progression differ between patients with spinal neoplasms and metastases and those with degenerative spine disease, both cohorts must be analysed separately. However, the study mentioned above included both patients with spinal neoplasms and those with degenerative spinal diseases. Moreover, interpretation of the findings of the meta-analysis was limited because the postoperative adverse events were not differentiated in detail, a synthesis of evidence on the patient-reported outcomes was not performed, and the method for the meta-analysis was not described clearly [17,18,19].
Two parameters help to identify frailty status. These include the frailty phenotype [20] and the frailty index (FI) [21]. Regarding the frailty phenotype, frailty is determined by the following symptoms: unintentional weight loss, self-reported exhaustion, weakness, slow walking speed, and low physical activity [20]. The FI is obtained by dividing the sum of a patient’s deficits by the total sum of frailty-related deficits. It has two types, namely adult spinal deformity (ASD)-FI [13] and cervical deformity (CD)-FI [22]. Recently, modified FI (mFI) has also been used for determining frailty [23]; each clinical institution has developed and used a different frailty tool [24]. Determining the risk stratification of frailty before spine surgery helps determine the prognosis and treatment of patients. Thus, we aimed to explore the following: (1) tools used to measure the frailty of patients prior to surgery for degenerative spine disease, (2) types of frailty-related health-related outcomes following spine surgery, and (3) association between preoperative frailty and health-related outcomes.
Methods
We followed the recommendations of the Cochrane Handbook to confirm the outcome of frailty [25]. The final protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO; registration number: CRD42021286341).
Search strategy
Electronic bibliographic databases, including Ovid-MEDLINE, Ovid-EMBASE, Cochrane Library (Cochrane Database of Systematic Reviews), and CINAHL (Cumulative Index of Nursing and Allied Health), were screened for relevant articles. The search terms were “spine,” “frailty,” “postoperative,” and “outcome” and the Boolean operators OR and were used to combine them. The search was completed on July 16, 2022. The search strategies for each database are presented in Supplementary Material Table 1.
Eligibility criteria
The inclusion criteria were as follows: (1) articles on patients who underwent spine surgery; (2) articles on studies that compared health-related outcomes (COs and PROs) after spine surgery with respect to preoperative frailty status, (3) articles in English published in peer-reviewed journals; and (4) articles on prospective or retrospective cohort, case-control, and cross-sectional studies. The exclusion criteria were as follows: (1) reviews, case reports, and unpublished manuscripts; (2) articles on studies that included spinal tumours; (3) articles on experimental studies (interventions could confound the relationship between frailty and postoperative health-related outcomes); (4) articles on studies that included non-surgical procedures. No restrictions were placed on the timing of publication.
Article selection and data extraction
Articles were first downloaded using reference management software (EndNote version 20, Clarivate Analytics, USA). Then, Rayyan was used to screen the downloaded articles and remove any duplicates [26]. Two authors (WB and YK) independently read the titles and abstracts of the remaining articles and selected those that met the eligibility criteria. Thereafter, the full texts of the selected articles were reviewed; any discrepancies in the selection process were resolved after discussion with another author (SP). Using a standardized record extraction form, the two aforementioned reviewers independently extracted the following data from the selected articles: first author’s name, year and country of publication, demographic and clinical characteristics of the study population, population demographics, type of surgery, measurement tool and outcomes, and follow-up duration.
Risk of bias in individual studies
The Risk of Bias Assessment Tool for Nonrandomized Studies (RoBANS) was used to assess the quality of the included studies [27]. The RoBANS evaluated the risk of bias for the following six domains: participant selection, confounding variables, measurement of exposure, blinding of outcome assessments, incomplete outcome data, and selective outcome reporting. Each domain was assessed as having a “low risk of bias”, “unclear risk of bias,” or “high risk of bias.” The two aforementioned authors independently evaluated the methodological quality of the studies and later combined their findings.
Synthesis and statistical analysis
All data analyses were performed using R (version 4.0.3, R Foundation for Statistical Computing, Austria). We performed a qualitative synthesis to determine what tools were used to measure frailty in patients undergoing spine surgery and what indicators were used for frailty and health-related outcomes. Thereafter, quantitative synthesis was performed to confirm the direction and magnitude of the association between frailty and health-related outcomes.
We divided the postoperative health-related outcomes into COs and PROs. The meta-analysis was performed if the following conditions were met: (1) there were three or more papers that could be synthesized, (2) the participants could be divided into frail and non-frail groups, (3) COs were synthesized only if the terms used in each paper were identical, and (4) the same participants were extracted from the same database in the same year (the paper that was published first was selected).
The Mantel–Haenszel method was used to estimate the pooled odds ratio (OR) with the 95% confidence interval (CI) for dichotomous variables. The inverse variance method was used to estimate the pooled mean difference (MD) with the 95% CI for continuous variables. A fixed-effect model was used for homogeneous studies, while a random-effects model was used for heterogeneous studies [25]. The I2 value was used to investigate the heterogeneity among the included studies; an I2 value > 50% was considered indicative of substantial heterogeneity [28].
Because tests for publication bias need to be evaluated when there are more than 10 studies in a meta-analysis, statistical tests were not attempted to identify publication bias in our study. Sensitivity analysis was performed while excluding papers that were judged to increase the heterogeneity and cause a bias in the effect size in the meta-analysis [25]. Statistical significance was defined by p-value < 0.05.
Results
Study selection
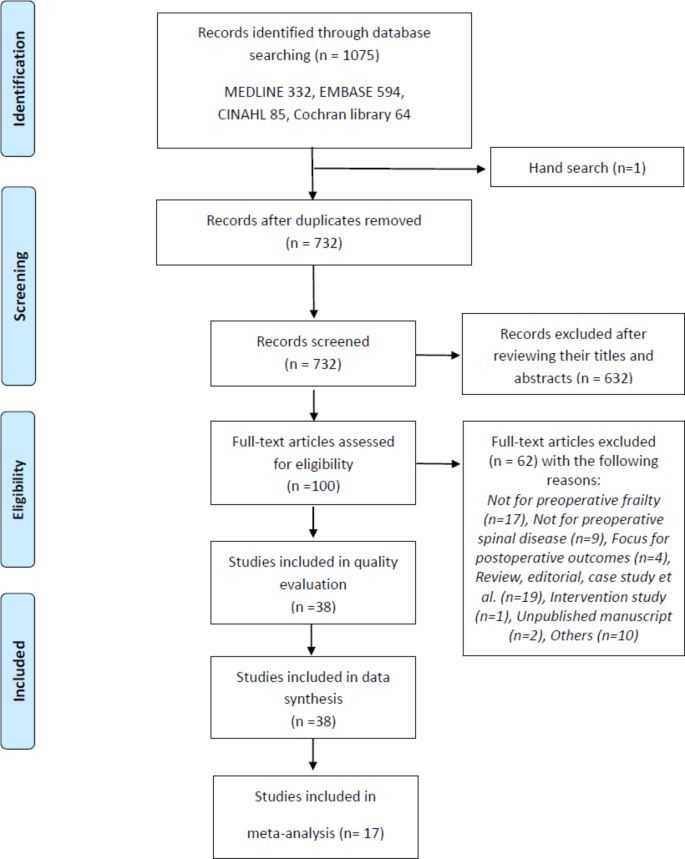
The study selection process is shown in Fig. 1. The initial search of the databases yielded 1,075 potentially relevant articles; one additional article was identified from other sources [29]. Among these, 732 articles remained after the removal of duplicates. After screening their titles and abstracts, 632 of these articles were excluded. The full texts of the remaining 100 articles were reviewed, and 62 articles were further excluded. The remaining 38 articles were finally included for quality evaluation and qualitative synthesis [7, 10,11,12,13,14, 16, 22,23,24, 29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56]. Among these, 17 were subjected to a quantitative synthesis for the meta-analysis [10, 13, 16, 22, 29, 30, 33, 35, 39,40,41,42, 47, 49, 52, 55, 56].
Study characteristics
The characteristics of the included studies are presented in Table 1. The countries of the patients who participated in the study were North America (n = 25) [7, 10,11,12,13,14, 22,23,24, 29, 31, 32, 37, 40,41,42,43,44,45, 47,48,49, 51,52,53, 56], Korea (n = 5) [30, 33,34,35,36], China (n = 2) [16, 50], Europe (n = 2) [38, 46], Japan (n = 2) [54, 55]. One study included patients from Europe, Asia, and North America [39]. Overall, 34 retrospective cohort studies [7, 10, 13, 14, 16, 22,23,24, 29, 31,32,33,34,35,36,37,38, 40,41,42,43,44,45,46,47, 49,50,51,52,53,54,55,56], 3 prospective cohort studies [11, 30, 39, 48], and 1 mixed retrospective and prospective cohort study [12] were included. The articles were published between 2016 and 2022. Overall, the studies comprised 474,651 patients who underwent spine surgery (mean age: 56.6–78.3 years).
Risk of bias
Supplementary Material Fig. 1 summarizes the results of the assessments of the risk of bias in the included studies. The overall quality of the included studies was good. However, there were concerns regarding selection bias for six out of 38 studies [23, 29, 36, 45,46,47]. These studies analysed multi-centre data and had a retrospective design, but did not report the confounding variables. Eleven studies [10, 14, 16, 22, 23, 29, 34, 35, 40, 52, 53] did not report the presence of incomplete outcome data, such as missing data or non-response rates. In more than 80% of the studies, five of the six evaluated domains were assessed as having a low risk of bias (attrition bias was excluded). No studies were excluded based on quality assessment.
Frailty measurements
The measurement tools for preoperative frailty included the mFI-11 (n = 15) [10, 12, 16, 23, 30, 32, 33, 35, 41, 44, 49, 50, 53,54,55], mFI-5 (n = 10) [7, 30, 31, 34, 44, 45, 52, 53, 55, 56], ASD-FI (n = 6) [13, 37,38,39, 42, 47], Hospital Frailty Risk Score (n = 2) [14, 46], Johns Hopkins Adjusted Clinical Groups indicator (n = 2) [24, 51], mCD-FI (n = 2) [29, 43], frailty phenotype (n = 3) [11, 36, 48], CD-FI (n = 1) [22], comprehensive geriatric assessment (n = 1) [30], and mASD-FI (n = 1) [40]. In these studies, the patients were divided into non-frail, prefrail, frail, or severely frail groups or into the low frailty, medium frailty, and high frailty groups, according to their criteria.
Health-related outcomes after spine surgery
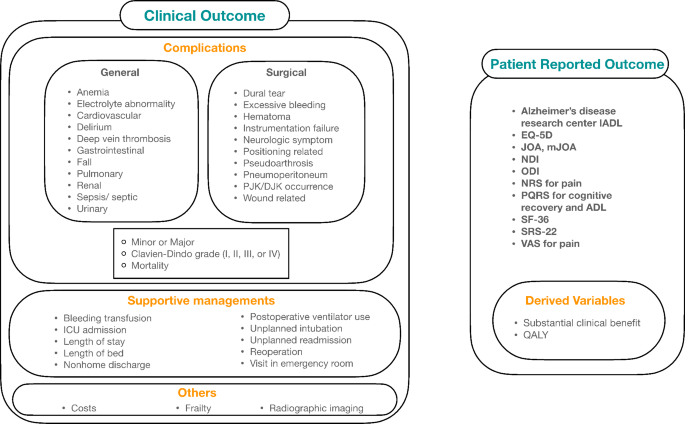
In the included studies, postoperative health-related outcomes were classified into COs and PROs (Table 1; Fig. 2, and Supplementary Material Table 2).
Health-related outcomes in terms of preoperative frailty status. IADL, instrumental activities of daily living; EQ-5D, EuroQol-5D; JOA, Japanese orthopedic association scale; mJOA, modified Japanese orthopedic association scale; NDI, neck disability index; ODI, Owestry disability index; NRS, numerical rating scale; PQRS, postoperative quality of recovery scale; ADL, activity of daily living; SF-36, 36-item short-form survey; SRS-22, Scoliosis Research Society 22-question; VAS, visual analog scale; QALY, quality-adjusted life years; ICU, intensive care unit
Clinical outcomes
All studies, except one [47], considered COs as postoperative health-related outcomes. The COs included postoperative complications and supportive management procedures.
In 35 studies, the postoperative complications were addressed as COs [7, 10,11,12, 14, 16, 22,23,24, 29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46, 49,50,51,52,53,54,55,56]. The postoperative complications were further divided into general and surgical complications. The general complications comprised anaemia; electrolyte abnormalities; cardiovascular, gastrointestinal, pulmonary, renal, and urinary complications; delirium; deep vein thrombosis; falls; and sepsis/septic shock. The surgical complications comprised dural tears, excessive bleeding, hematomas, instrumentation failure, neurological symptoms, positional and wound-related complications, pseudoarthrosis, pneumoperitoneum, and kyphosis. These complications were classified as minor or major or I–IV (Clavien–Dindo classification) [57]. In five studies [16, 22, 37,38,39], the definition provided by Glassman et al. was used to determine the major complications [58, 59]. In 13 studies [10, 12, 23, 24, 29, 32, 35, 41, 44, 49, 50, 52, 53], mortality was considered a postoperative complication.
Supportive management procedures included transfusion for bleeding [10, 41, 46, 52], admissions to intensive care units [14, 22], length of hospital stay [11, 12, 14, 22, 24, 29, 31,32,33, 36,37,38,39,40,41,42, 45, 50, 53, 56], length of bed rest [33], nonhome discharge [7, 11, 12, 14, 22, 24, 29, 32, 50,51,52,53, 56], postoperative ventilator use [52], reintubation [35, 52, 56], readmission [7, 14, 24, 31, 44, 50, 52, 53, 56], reoperation [7, 10, 29, 31, 33, 37, 38, 40, 41, 43, 46, 50, 53], and emergency room visit [14].
Other COs included costs [13, 14, 24, 51], frailty status [48], and radiographic imaging findings [13, 16, 43, 54].
Patient reported outcomes
Eleven studies assessed PROs [13, 16, 29, 33, 40, 42, 43, 47, 48, 50, 54]. The PROs were assessed using the instrumental activities of daily living [48], EuroQol-5D (EQ-5D) [13, 29, 40], Japanese Orthopaedic Association (JOA) score [16], modified mJOA score [43], Neck Disability Index [29, 43], Oswestry Disability Questionnaire (ODI) [13, 16, 33, 40, 42, 47, 50, 54], numerical rating scale for pain [29, 42, 43, 47], Postoperative Quality of Recovery Scale for cognitive recovery and activities of daily living [48], Pain Catastrophizing Scale [40], 36-Item Short Form Survey (SF-36) [47, 50, 54], Scoliosis Research Society 22-question [16, 40, 42, 54], and visual analogue scale for pain [16, 33, 54].
Substantial clinical benefit was determined based on changes in the ODI, SF-36 score, and back and leg pain score after the surgery [33, 47]. The quality-adjusted life years were determined using the EQ-5D [13].
Meta-analysis of the selected outcomes
Synthesis of meta-analysis results regarding the clinical outcomes
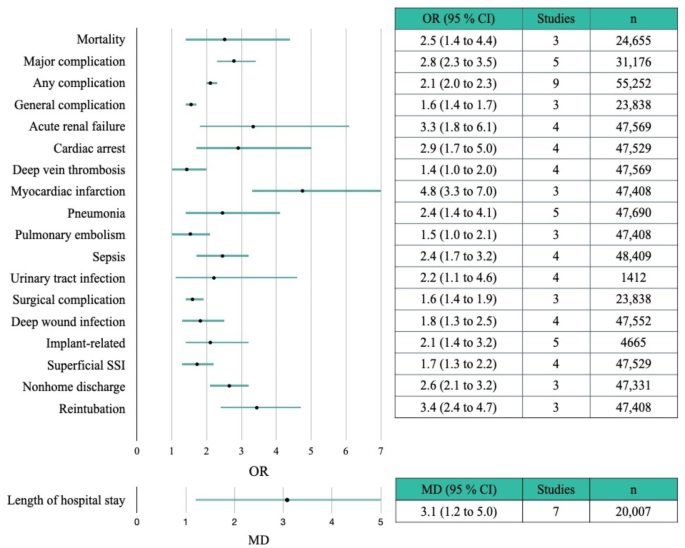
Results of the meta-analysis of the COs are presented in Table 2. A forest plot depicting significant associations between COs and frailty is shown in Fig. 3. Compared to the non-frail group, the frail group was more likely to experience the following COs: mortality (OR = 2.5; 95% CI = 1.4–4.4) [10, 35, 52], major complication (OR = 2.8; 95% CI = 2.3–3.5) [39, 42, 49, 56], any complication (OR = 2.1; 95% CI = 2.0–2.3) [10, 29, 35, 39, 40, 42, 52, 55, 56], general complication (OR = 1.6; 95% CI = 1.4–1.7) [22, 30, 52], acute renal failure (OR = 3.3; 95% CI = 1.8–6.1) [16, 35, 52, 56], cardiac arrest (OR = 2.9; 95% CI = 1.7–5.0) [29, 35, 52, 56], deep vein thrombosis (OR = 1.4; 95% CI = 1.0–2.0) [16, 35, 52, 56], gastrointestinal complication (OR = 0.9; 95% CI = 0.4–1.9) [16, 29, 33, 42], myocardial infarction (OR = 4.8; 95% CI = 3.3–7.0) [35, 52, 56], pneumonia (OR = 2.4; 95% CI = 1.4–4.1) [16, 29, 35, 52, 56], pulmonary embolism (OR = 1.5; 95% CI = 1.0–2.1) [35, 52, 56], sepsis (OR = 2.4; 95% CI = 1.7–3.2) [10, 35, 52, 56], stroke/cerebrovascular accident (OR = 2.1; 95% CI = 0.5–8.5) [16, 35, 41], urinary tract infection (OR = 2.2; 95% CI = 1.1–4.6) [10, 29, 33, 35], surgical complication (OR = 1.6; 95% CI = 1.4–1.9) [22, 30, 52], deep wound infection (OR = 1.8; 95% CI = 1.3–2.5) [16, 29, 52, 56], implant-related complication (OR = 2.1; 95% CI = 1.4–3.2) [29, 33, 41, 42, 55], neurological complication (OR = 1.1; 95% CI = 0.6–1.7) [16, 29, 33, 41, 42], superficial surgical site infection (OR = 1.7; 95% CI = 1.3–2.2) [29, 35, 52, 56], length of stay (MD = 3.1; 95% CI = 1.2–5.0) [13, 16, 24, 33, 37, 38, 51], non-home discharge (OR = 2.6; 95% CI = 2.1–3.2) [22, 52, 56], reintubation (OR = 3.4; 95% CI = 2.4–4.7) [35, 52, 56], and reoperation (OR = 1.0; 95% CI = 0.4–2.5) [10, 29, 33, 52]. The forest plot for each CO is presented in Supplementary Material Fig. 2.
The incidence rates of complications in the frail group and the robust group are presented in Supplementary Table 3. In the robust group, the five most prevalent complications, in descending order, were as follows: gastrointestinal complications (5.6%), urinary tract infection (4.6%), implant-related complications (1.5%), neurological complications (1.4%), and superficial surgical site infections (0.6%). In contrast, in the frail group, the five most prevalent complications, in descending order, were as follows: implant-related complications (21.5%), neurological complications (13.6%), urinary tract infections (9.3%), gastrointestinal complications (5.6%), and stroke/cerebrovascular accidents (2.1%).
Synthesis of meta-analysis results regarding the patient-reported outcomes
Results of the meta-analysis of the PROs are presented in Table 2. A forest plot for the PROs is shown in Supplementary Material Fig. 3. Changes in the ODI scores between pre- and post-surgery, categorized by frailty, were synthesized based on three papers [13, 16, 47]. The changes between pre- and post-operative ODI scores were not associated with preoperative frailty (MD= -9.6, 95% CI= -23–3.8).
Sensitivity analysis
A sensitivity analysis was performed to identify the relationship between any complication and frailty, which had the highest number of synthesized papers. As shown in the forest plot for any complication (Supplementary Material Figs. 2 and 3), it was judged that heterogeneity occurred due to the articles by Passias et al. [29] and Kim et al. [35]. When a meta-analysis was performed by removing those two articles, the I2 value was reduced to 53% and 47%, respectively (Supplementary Material Fig. 4). Therefore, after removing these two papers, the meta-analysis was performed again (Supplementary Material Fig. 5). A fixed-effect model was selected because the heterogeneity was reduced to 10% for I2. The OR for any complication was 2.1 (95% CI = 2.0–2.3), which did not differ significantly from the original OR of 2.1. The findings of the sensitivity analysis indicate that the results of this study are reliable.
Discussion
This systematic review and meta-analysis examined the association between preoperative frailty and postoperative health-related outcomes in patients who underwent spine surgery for degenerative spinal disease. In the 38 included studies, 10 frailty instruments were used to measure preoperative frailty and two typologies of health-related outcomes for the preoperative frailty status were identified. Preoperative frailty was observed to be associated with postoperative adverse health-related outcomes. It increased the incidence of adverse COs, including mortality and complications, but there was no significant difference with respect to the improvement of the postoperative PROs.
Research on frailty has increased appreciably recently; this includes studies on preoperative frailty and its association with COs [15, 60] or PROs [61] and studies on the construct validity of frailty instruments [62]. Previous studies conducted in surgical settings highlight the important role of frailty as a prognostic factor for considering surgery [15, 60, 61, 63]. A systematic review and meta-analysis of 19 studies on patients undergoing cardiac surgery revealed that frailty was associated with a two-fold greater risk of mortality, greater complications, and five-fold greater risk of non-home discharge [60]. In another systematic review and meta-analysis of 71 studies on adult patients undergoing cancer surgery, frailty was found to be related to a three-fold, two-fold, and four-fold greater risk of 30-day mortality, postoperative complications, and long-term mortality, respectively [15]. Our findings corroborate and extend the existing evidence on the association of preoperative frailty with postoperative adverse COs.
Factors other than age should be considered when predicting postoperative recovery in patients with degenerative spinal diseases [17, 20]. The prevalence of frailty is increasing among individuals undergoing spine surgeries. Analysis of a patient population that underwent spine surgery, using data from the American College of Surgeons National Surgical Quality Improvement Program database, revealed that the number of frail patients doubled from 2005 to 2016 [44]. This suggests that frailty is an important variable to consider for risk stratification when predicting postoperative recovery in patients with degenerative spinal disease [17, 20]. The frailty score may serve as a preoperative screening tool to aid in decision-making and perioperative management. It can help monitor patients’ health, thereby allowing healthcare professionals to identify high-risk patients and develop better treatment strategies. It can also help guide discussions among healthcare professionals, patients, and family members to reduce surgical vulnerability, enable pre-habilitation to increase patient resilience, and customize perioperative care [64, 65].
In our qualitative synthesis, clinical outcomes were identified as health-related outcomes in all but one study [47]. Postoperative complications can be divided into general and surgery-related complications. Supportive management strategies include blood transfusions and unplanned intubations; these represent additional supportive care provided to patients with problems that are not part of the normal recovery process.
Among the COs in this study, 19 items were synthesized for quantitative analysis, and 3–9 studies participated in the synthesis. If there are fewer than 10 studies, statistical confirmatory tests for publication bias (e.g. the funnel test) are not recommended [25]; thus, publication bias could not be confirmed in this study. Therefore, items that showed heterogeneity, such as any complications, pneumonia, length of hospital stay, non-home discharge, and reoperation, should be interpreted carefully. In case of any complications, a sensitivity analysis was performed because the number of studies was considerably large and heterogeneity was noted across the studies. This analysis identified two studies as outliers [29, 35], and the synthesis was attempted again by excluding them. The re-analysis revealed that the heterogeneity improved and the effect size did not affect the existing results.
The meta-analysis of the clinical outcomes in this study revealed that the risk of mortality in the frail group was 2.5 times higher than that in the non-frail group. Furthermore, the probability of major complication, any complication, general complication, acute renal failure, cardiac arrest, deep vein thrombosis, myocardial infarction, pneumonia, pulmonary embolism, sepsis, stroke/cerebrovascular accident, surgical complication, deep-wound infection, implant-related complication, superficial surgical site infection, length of hospital stay, nonhome discharge, and reintubation was higher in the frail group than in the non-frail group. Notably, the order of complication prevalence was different between the robust and frail groups. In the robust group, the most common complication was relatively simple gastrointestinal complications, while in the frail group, relatively severe implant-related complications, which might necessitate reoperation, were the most common. The increased incidence of complications or the severity of complications in frail patients can be attributed to several factors. Frailty is linked to reduced immune function, which can result in compromised ability to cope with complications such as infections during the stress of post-surgery recovery [66]. Frailty is associated with decreased metabolic activity, such as high levels of glucose and LDL cholesterol, which can impair tissue nutrient supply and metabolic functions [67], ultimately hindering post-surgery recovery capacity. Furthermore, frailty is associated with low physical activity levels and reduced muscle mass [66, 68], which might persist post-surgery, leading to compromised recovery due to limited physical activity. Healthcare professionals who deliver postoperative care to frail patients should be aware of these complications. This can lead to increases in the time of direct nursing care and the cost of physical resources such as ICU and rehabilitation, as well as convalescent care beds [69].
Another key knowledge gap that thwarts a more meaningful prognosis is the lack of data on PROs. Studies have paid considerable attention to frailty as an important preoperative risk indicator for COs [15, 61]; similar studies for PROs are few. Data on cognitive outcomes, functional outcomes, and quality of life are lacking. In our systematic review, only 11 of 38 studies reported the effects of frailty on the PROs (e.g., quality of life, ODI, and pain); the multidimensional health status of patients was reported in just six studies [13, 29, 40, 47, 50, 54]. The wide variety of outcome measures limited the comparison of results among the included studies. The meta-analysis revealed that frailty was not significantly associated with the postoperative ODI and changes in the perioperative ODI; however, it had a conflicting relationship with the COs. Specifically, compared to non-frail patients, frail patients experienced greater improvements in ODI, quality of life, and pain [47]. Such improvements are partly explained by corrections in postural deformity, as frail patients have worse preoperative sagittal imbalances than those who do not [70, 71]. When choosing the best treatment options for patients with degenerative spinal diseases, it is necessary to consider their preferences and values [72, 73]. Frailty assessment can help patients and their families make informed decisions before surgery. It highlights the need for future studies to determine the association between frailty and PROs in patients with degenerative spinal disease.
We identified the typologies of postoperative health-related outcomes associated with preoperative frailty in patients who underwent spine surgery for degenerative spinal disease. These typologies can inform the content and structure of pre-rehabilitation and customized educational programs for patients undergoing spine surgery. They can also be used as basic data for implementing programs or pathways to reverse frailty in patients with spinal diseases and improve their health-related outcomes. Furthermore, the identified typologies can help develop evaluation tools to evaluate frailty-associated health-related outcomes in patients undergoing spine and other surgeries.
Finally, frailty is an important prognostic marker for postoperative health-related outcomes in patients with degenerative spinal disease, but there is a lack of consensus on the best means to accurately and efficiently determine frailty in patients undergoing spine surgery. In this review and meta-analysis, 10 different frailty instruments (including the mFI-5, mFI-11, and ASD-FI) were used to define frailty, and the variability in the evaluations by the same tool was demonstrated. A review of 14 different tools used for the assessment of frailty in a population undergoing spine surgery (age: >18 years) revealed wide variabilities in the tool components, time required to complete the assessment, and efficacy of outcome prediction among the tools [74]. Furthermore, significant heterogeneity was observed among the tools with respect to the cut-off values for risk establishment and stratification. In acute care hospitals, it is difficult to determine the most suitable tool for clinical practice. Future studies must prospectively validate frailty tools to confirm their effectiveness and applicability as reliable risk-stratification tools for the diagnosis of frailty among patients with degenerative spinal disease.
This study has some limitations. First, a meta-analysis of some items could not be performed due to data heterogeneity. Specifically, although all patients underwent spine surgery, the severity of the surgery differed among the studies because of a mixture of fusion and decompression. Furthermore, the detection of COs differed due to a mixture of prospective and retrospective studies. There were inconsistencies among the studies in the definition of frailty and the scales used for frailty analysis. Furthermore, there was heterogeneity among the frailty tools used. Second, only less than half of the included studies were included in the meta-analyses due to insufficient data (e.g., some studies reported only comparing ratios; for the same patient in the same database, only the first studies published first were considered). Third, because there were few than 10 studies in our meta-analysis, we could not identify or evaluate publication bias.
The number of patients undergoing spine surgery for degenerative spinal diseases is increasing. Thus, despite the aforementioned limitations, our study is of high clinical value because it evaluated the effects of frailty on the health-related outcomes of these patients. Our findings can guide future studies and aid healthcare professionals who treat patients with degenerative spinal diseases.
Conclusion
This systematic review and meta-analysis identified frailty as a strong predictor of COs in patients after spine surgery; however, preoperative frailty and PROs are still inconclusive. Further studies are needed to investigate the association between frailty and PROs. With the increasing number of frail patients undergoing spine surgery for degenerative spinal diseases, healthcare professionals should be aware of the effects of frailty and develop improved and focused perioperative management strategies for stratified frail patients. In particular, the development of interventions comprising treatment goals and plans that consider preoperative frailty as a risk factor for mortality and poor functional recovery can be an important cornerstone of preoperative management. Future research should focus on the development and implementation of interventions that could potentially improve postoperative cognitive, functional, and adverse outcomes in frail patients undergoing spine surgery.
Data Availability
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Abbreviations
- CO:
-
Clinical outcomes
- PRO:
-
Patient-reported outcome
- FI:
-
Frailty index
- mFI:
-
Modified frailty index
- ASD:
-
Adult spinal deformity
- CD:
-
Cervical deformity
- RoBANS:
-
The Risk of Bias Assessment Tool for Nonrandomized Studies
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- MD:
-
Mean difference
- EQ-5D:
-
EuroQol-5D
- JOA:
-
Japanese Orthopaedic Association
- ODI:
-
Oswestry Disability Questionnaire
- SF-36:
-
36-Item Short Form Survey
References
Yolcu YU, Helal A, Alexander AY, Bhatti AU, Alvi MA, Abode-Iyamah K, Bydon M. Minimally invasive Versus Open Surgery for degenerative spine disorders for Elderly patients: experiences from a single Institution. World Neurosurg. 2021;146:e1262–9. https://doi.org/10.1016/j.wneu.2020.11.145.
Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in lumbar Fusion Procedure Rates and Associated Hospital costs for degenerative spinal Diseases in the United States, 2004 to 2015. Spine (Phila Pa 1976). 2019;44(5):369–76. https://doi.org/10.1097/brs.0000000000002822.
Beschloss A, Dicindio C, Lombardi J, Varthi A, Ozturk A, Lehman R, Lenke L, Saifi C. Marked increase in spinal deformity Surgery throughout the United States. Spine (Phila Pa 1976). 2021;46(20):1402–8. https://doi.org/10.1097/brs.0000000000004041.
Kobayashi K, Ando K, Nishida Y, Ishiguro N, Imagama S. Epidemiological trends in spine Surgery over 10 years in a multicenter database. Eur Spine J. 2018;27(8):1698–703. https://doi.org/10.1007/s00586-018-5513-4.
Neifert SN, Martini ML, Yuk F, McNeill IT, Caridi JM, Steinberger J, Oermann EK. Predicting trends in cervical spinal Surgery in the United States from 2020 to 2040. World Neurosurg. 2020;141:e175–81. https://doi.org/10.1016/j.wneu.2020.05.055.
Puvanesarajah V, Jain A, Kebaish K, Shaffrey CI, Sciubba DM, De la Garza-Ramos R, Khanna AJ, Hassanzadeh H. Poor Nutrition status and lumbar Spine Fusion Surgery in the Elderly: readmissions, Complications, and Mortality. Spine (Phila Pa 1976). 2017;42(13):979–83. https://doi.org/10.1097/brs.0000000000001969.
Chan V, Witiw CD, Wilson JR, Wilson JR, Coyte P, Fehlings MG. Frailty is an important predictor of 30-day morbidity in patients treated for lumbar spondylolisthesis using a posterior surgical approach. Spine J. 2021. https://doi.org/10.1016/j.spinee.2021.08.008.
Hirase T, Haghshenas V, Bratescu R, Dong D, Kuo PH, Rashid A, Kavuri V, Hanson DS, Meyer BC, Marco RAW. Sarcopenia predicts perioperative adverse events following complex revision Surgery for the thoracolumbar spine. Spine J. 2021;21(6):1001–9. https://doi.org/10.1016/j.spinee.2021.02.001.
Hanna K, Ditillo M, Joseph B. The role of frailty and prehabilitation in Surgery. Curr Opin Crit Care. 2019;25(6):717–22. https://doi.org/10.1097/mcc.0000000000000669.
Leven DM, Lee NJ, Kothari P, Steinberger J, Guzman J, Skovrlj B, Shin JI, Caridi JM, Cho SK. Frailty Index is a significant predictor of Complications and mortality after Surgery for adult spinal deformity. Spine (Phila Pa 1976). 2016;41(23):E1394–e1401. https://doi.org/10.1097/brs.0000000000001886.
Susano MJ, Grasfield RH, Friese M, Rosner B, Crosby G, Bader AM, Kang JD, Smith TR, Lu Y, Groff MW, et al. Brief preoperative screening for Frailty and Cognitive Impairment predicts delirium after spine Surgery. Anesthesiology. 2020;133(6):1184–91. https://doi.org/10.1097/aln.0000000000003523.
Charest-Morin R, Street J, Zhang H, Roughead T, Ailon T, Boyd M, Dvorak M, Kwon B, Paquette S, Dea N, et al. Frailty and Sarcopenia do not predict adverse events in an elderly population undergoing non-complex primary elective Surgery for degenerative conditions of the lumbar spine. Spine J. 2018;18(2):245–54. https://doi.org/10.1016/j.spinee.2017.07.003.
Brown AE, Lebovic J, Alas H, Pierce KE, Bortz CA, Ahmad W, Naessig S, Hassanzadeh H, Labaran LA, Puvanesarajah V, et al. A cost utility analysis of treating different adult spinal deformity frailty states. J Clin Neurosci. 2020;80:223–8. https://doi.org/10.1016/j.jocn.2020.07.047.
Hannah TC, Neifert SN, Caridi JM, Martini ML, Lamb C, Rothrock RJ, Yuk FJ, Gilligan J, Genadry L, Gal JS. Utility of the Hospital Frailty Risk score for Predicting adverse outcomes in degenerative spine Surgery cohorts. Neurosurgery. 2020;87(6):1223–30. https://doi.org/10.1093/neuros/nyaa248.
Shaw JF, Budiansky D, Sharif F, McIsaac DI. The Association of Frailty with outcomes after Cancer Surgery: a systematic review and metaanalysis. Ann Surg Oncol. 2022. https://doi.org/10.1245/s10434-021-11321-2.
Li B, Meng X, Zhang X, Hai Y. Frailty as a risk factor for postoperative Complications in adult patients with degenerative scoliosis administered posterior single approach, long-segment corrective Surgery: a retrospective cohort study. BMC Musculoskelet Disord. 2021;22(1):333. https://doi.org/10.1186/s12891-021-04186-9.
Chan V, Wilson JRF, Ravinsky R, Badhiwala JH, Jiang F, Anderson M, Yee A, Wilson JR, Fehlings MG. Frailty adversely affects outcomes of patients undergoing spine Surgery: a systematic review. Spine J. 2021;21(6):988–1000. https://doi.org/10.1016/j.spinee.2021.01.028.
Handforth C, Clegg A, Young C, Simpkins S, Seymour MT, Selby PJ, Young J. The prevalence and outcomes of frailty in older cancer patients: a systematic review. Ann Oncol. 2015;26(6):1091–101. https://doi.org/10.1093/annonc/mdu540.
Dai S, Yang M, Song J, Dai S, Wu J. Impacts of Frailty on Prognosis in Lung Cancer patients: a systematic review and Meta-analysis. Front Med (Lausanne). 2021;8:715513. https://doi.org/10.3389/fmed.2021.715513.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–156. https://doi.org/10.1093/gerona/56.3.m146.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–95. https://doi.org/10.1503/cmaj.050051.
Miller EK, Ailon T, Neuman BJ, Klineberg EO, Mundis GM Jr., Sciubba DM, Kebaish KM, Lafage V, Scheer JK, Smith JS, et al. Assessment of a Novel Adult Cervical deformity Frailty Index as a component of preoperative risk stratification. World Neurosurg. 2018;109:e800–6. https://doi.org/10.1016/j.wneu.2017.10.092.
Ali R, Schwalb JM, Nerenz DR, Antoine HJ, Rubinfeld I. Use of the modified frailty index to predict 30-day morbidity and mortality from spine Surgery. J Neurosurg Spine. 2016;25(4):537–41. https://doi.org/10.3171/2015.10.Spine14582.
Shahrestani S, Ton A, Chen XT, Ballatori AM, Wang JC, Buser Z. The influence of frailty on postoperative Complications in geriatric patients receiving single-level lumbar fusion Surgery. Eur Spine J. 2021;30(12):3755–62. https://doi.org/10.1007/s00586-021-06960-8.
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane handbook for systematic reviews of interventions version 6.3. (updated Feburary 2022). In.: Cochrane Handbook; 2022.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. https://doi.org/10.1186/s13643-016-0384-4.
Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, Jang BH, Son HJ. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013;66(4):408–14. https://doi.org/10.1016/j.jclinepi.2012.09.016.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557.
Passias PG, Bortz CA, Segreto FA, Horn SR, Lafage R, Lafage V, Smith JS, Line B, Kim HJ, Eastlack R, et al. Development of a modified cervical deformity Frailty Index: a Streamlined Clinical Tool for Preoperative Risk Stratification. Spine (Phila Pa 1976). 2019;44(3):169–76. https://doi.org/10.1097/brs.0000000000002778.
Chang SY, Son J, Park SM, Chang BS, Lee CK, Kim H. Predictive Value of Comprehensive Geriatric Assessment on early postoperative Complications following lumbar spinal stenosis Surgery: a prospective cohort study. Spine (Phila Pa 1976). 2020;45(21):1498–505. https://doi.org/10.1097/brs.0000000000003597.
Elsamadicy AA, Freedman IG, Koo AB, David WB, Reeves BC, Havlik J, Pennington Z, Kolb L, Shin JH, Sciubba DM. Modified-frailty index does not independently predict Complications, hospital length of stay or 30-day readmission rates following posterior lumbar decompression and fusion for spondylolisthesis. Spine J. 2021;21(11):1812–21. https://doi.org/10.1016/j.spinee.2021.05.011.
Flexman AM, Charest-Morin R, Stobart L, Street J, Ryerson CJ. Frailty and postoperative outcomes in patients undergoing Surgery for degenerative spine Disease. Spine J. 2016;16(11):1315–23. https://doi.org/10.1016/j.spinee.2016.06.017.
Jung JM, Chung CK, Kim CH, Yang SH, Ko YS. The modified 11-Item Frailty Index and postoperative outcomes in patients undergoing lateral lumbar Interbody Fusion. Spine (Phila Pa 1976). 2022;47(5):396–404. https://doi.org/10.1097/brs.0000000000004260.
Kang T, Park SY, Lee JS, Lee SH, Park JH, Suh SW. Predicting postoperative Complications in patients undergoing lumbar spinal fusion by using the modified five-item frailty index and nutritional status. Bone Joint J. 2020;102–b(12):1717–22. https://doi.org/10.1302/0301-620x.102b12.Bjj-2020-0874.R1.
Kim JY, Park IS, Kang DH, Lee YS, Kim KT, Hong SJ. Prediction of risk factors after spine Surgery in patients aged > 75 years using the modified Frailty Index. J Korean Neurosurg Soc. 2020;63(6):827–33. https://doi.org/10.3340/jkns.2020.0019.
Kim DU, Park HK, Lee GH, Chang JC, Park HR, Park SQ, Cho SJ. Central Sarcopenia, Frailty and Comorbidity as Predictor of Surgical Outcome in Elderly patients with degenerative spine Disease. J Korean Neurosurg Soc. 2021;64(6):995–1003. https://doi.org/10.3340/jkns.2021.0074.
Miller EK, Neuman BJ, Jain A, Daniels AH, Ailon T, Sciubba DM, Kebaish KM, Lafage V, Scheer JK, Smith JS, et al. An assessment of frailty as a tool for risk stratification in adult spinal deformity Surgery. Neurosurg Focus. 2017;43(6):E3. https://doi.org/10.3171/2017.10.Focus17472.
Miller EK, Vila-Casademunt A, Neuman BJ, Sciubba DM, Kebaish KM, Smith JS, Alanay A, Acaroglu ER, Kleinstück F, Obeid I, et al. External validation of the adult spinal deformity (ASD) frailty index (ASD-FI). Eur Spine J. 2018;27(9):2331–8. https://doi.org/10.1007/s00586-018-5575-3.
Miller EK, Lenke LG, Neuman BJ, Sciubba DM, Kebaish KM, Smith JS, Qiu Y, Dahl BT, Pellisé F, Matsuyama Y, et al. External validation of the adult spinal deformity (ASD) Frailty Index (ASD-FI) in the Scoli-RISK-1 patient database. Spine (Phila Pa 1976). 2018;43(20):1426–31. https://doi.org/10.1097/brs.0000000000002717.
Passias PG, Moattari K, Pierce KE, Passfall L, Krol O, Naessig S, Ahmad W, Schoenfeld AJ, Ahmad S, Singh V, et al. Performance of the modified adult spinal deformity Frailty Index (mASD-FI) in Preoperative Risk Assessment. Spine (Phila Pa 1976). 2022. https://doi.org/10.1097/brs.0000000000004342.
Phan K, Kim JS, Lee NJ, Somani S, Di Capua J, Kothari P, Leven D, Cho SK. Frailty is associated with morbidity in adults undergoing elective anterior lumbar interbody fusion (ALIF) Surgery. Spine J. 2017;17(4):538–44. https://doi.org/10.1016/j.spinee.2016.10.023.
Pierce KE, Passias PG, Alas H, Brown AE, Bortz CA, Lafage R, Lafage V, Ames C, Burton DC, Hart R, et al. Does patient Frailty Status Influence Recovery following spinal Fusion for adult spinal deformity? An analysis of patients with 3-Year follow-up. Spine (Phila Pa 1976). 2020;45(7):E397–e405. https://doi.org/10.1097/brs.0000000000003288.
Pierce KE, Passias PG, Daniels AH, Lafage R, Ahmad W, Naessig S, Lafage V, Protopsaltis T, Eastlack R, Hart R, et al. Baseline Frailty Status influences recovery patterns and outcomes following alignment correction of cervical deformity. Neurosurgery. 2021;88(6):1121–7. https://doi.org/10.1093/neuros/nyab039.
Pierce KE, Naessig S, Kummer N, Larsen K, Ahmad W, Passfall L, Krol O, Bortz C, Alas H, Brown A, et al. The five-item modified Frailty Index is predictive of 30-day postoperative Complications in patients undergoing spine Surgery. Spine (Phila Pa 1976). 2021;46(14):939–43. https://doi.org/10.1097/brs.0000000000003936.
Pierce KE, Kapadia BH, Bortz C, Alas H, Brown AE, Diebo BG, Raman T, Jain D, Lebovic J, Passias PG. Frailty Severity impacts Development of Hospital-acquired conditions in patients undergoing corrective Surgery for adult spinal deformity. Clin Spine Surg. 2021;34(7):E377–e381. https://doi.org/10.1097/bsd.0000000000001219.
Pulido LC, Meyer M, Reinhard J, Kappenschneider T, Grifka J, Weber M. Hospital frailty risk score predicts adverse events in spine Surgery. Eur Spine J. 2022;31(7):1621–9. https://doi.org/10.1007/s00586-022-07211-0.
Reid DBC, Daniels AH, Ailon T, Miller E, Sciubba DM, Smith JS, Shaffrey CI, Schwab F, Burton D, Hart RA, et al. Frailty and Health-Related Quality of Life Improvement following adult spinal deformity Surgery. World Neurosurg. 2018;112:e548–54. https://doi.org/10.1016/j.wneu.2018.01.079.
Rothrock RJ, Steinberger JM, Badgery H, Hecht AC, Cho SK, Caridi JM, Deiner S. Frailty status as a predictor of 3-month cognitive and functional recovery following spinal Surgery: a prospective pilot study. Spine J. 2019;19(1):104–12. https://doi.org/10.1016/j.spinee.2018.05.026.
Shin JI, Kothari P, Phan K, Kim JS, Leven D, Lee NJ, Cho SK. Frailty Index as a predictor of adverse postoperative outcomes in patients undergoing cervical spinal Fusion. Spine (Phila Pa 1976). 2017;42(5):304–10. https://doi.org/10.1097/brs.0000000000001755.
Sun W, Lu S, Kong C, Li Z, Wang P, Zhang S. Frailty and post-operative outcomes in the older patients undergoing elective posterior Thoracolumbar Fusion Surgery. Clin Interv Aging. 2020;15:1141–50. https://doi.org/10.2147/cia.S245419.
Ton A, Shahrestani S, Saboori N, Ballatori AM, Chen XT, Wang JC, Buser Z. The impact of frailty on postoperative Complications in geriatric patients undergoing multi-level lumbar fusion Surgery. Eur Spine J. 2022;31(7):1745–53. https://doi.org/10.1007/s00586-022-07237-4.
Weaver DJ, Malik AT, Jain N, Yu E, Kim J, Khan SN. The modified 5-Item Frailty Index: a concise and useful Tool for assessing the impact of Frailty on postoperative morbidity following elective posterior lumbar fusions. World Neurosurg. 2019. https://doi.org/10.1016/j.wneu.2018.12.168.
Wilson JRF, Badhiwala JH, Moghaddamjou A, Yee A, Wilson JR, Fehlings MG. Frailty is a better predictor than age of mortality and perioperative Complications after Surgery for degenerative cervical myelopathy: an analysis of 41,369 patients from the NSQIP database 2010–2018. J Clin Med. 2020;9(11). https://doi.org/10.3390/jcm9113491.
Yagi M, Fujita N, Okada E, Tsuji O, Nagoshi N, Tsuji T, Asazuma T, Nakamura M, Matsumoto M, Watanabe K. Impact of Frailty and Comorbidities on Surgical outcomes and Complications in adult spinal disorders. Spine (Phila Pa 1976). 2018;43(18):1259–67. https://doi.org/10.1097/brs.0000000000002596.
Yagi M, Michikawa T, Hosogane N, Fujita N, Okada E, Suzuki S, Tsuji O, Nagoshi N, Asazuma T, Tsuji T, et al. The 5-Item modified Frailty Index is predictive of severe adverse events in patients undergoing Surgery for adult spinal deformity. Spine (Phila Pa 1976). 2019;44(18):E1083–e1091. https://doi.org/10.1097/brs.0000000000003063.
Zreik J, Alvi MA, Yolcu YU, Sebastian AS, Freedman BA, Bydon M. Utility of the 5-Item modified Frailty Index for Predicting adverse outcomes following elective Anterior Cervical Discectomy and Fusion. World Neurosurg. 2021;146:e670–7. https://doi.org/10.1016/j.wneu.2020.10.154.
Dindo D, Demartines N, Clavien PA. Classification of Surgical Complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG. The impact of perioperative Complications on clinical outcome in adult deformity Surgery. Spine (Phila Pa 1976). 2007;32(24):2764–70. https://doi.org/10.1097/BRS.0b013e31815a7644.
Glassman SD, Alegre G, Carreon L, Dimar JR, Johnson JR. Perioperative Complications of lumbar instrumentation and fusion in patients with Diabetes Mellitus. Spine J. 2003;3(6):496–501. https://doi.org/10.1016/s1529-9430(03)00426-1.
Lee JA, Yanagawa B, An KR, Arora RC, Verma S, Friedrich JO. Frailty and pre-frailty in cardiac Surgery: a systematic review and meta-analysis of 66,448 patients. J Cardiothorac Surg. 2021;16(1):184. https://doi.org/10.1186/s13019-021-01541-8.
Bezzina K, Fehlmann CA, Guo MH, Visintini SM, Rubens FD, Wells GA, Mazzola R, McGuinty C, Huang A, Khoury L, et al. Influence of preoperative frailty on quality of life after cardiac Surgery: protocol for a systematic review and meta-analysis. PLoS ONE. 2022;17(2):e0262742. https://doi.org/10.1371/journal.pone.0262742.
Alkadri J, Hage D, Nickerson LH, Scott LR, Shaw JF, Aucoin SD, McIsaac DI. Anesth Analg. 2021;133(5):1094–106. https://doi.org/10.1213/ane.0000000000005595. A Systematic Review and Meta-Analysis of Preoperative Frailty Instruments Derived From Electronic Health Data.
Kennedy CA, Shipway D, Barry K. Frailty and emergency abdominal Surgery: a systematic review and meta-analysis. Surgeon. 2021. https://doi.org/10.1016/j.surge.2021.11.009.
Nidadavolu LS, Ehrlich AL, Sieber FE, Oh ES. Preoperative evaluation of the Frail patient. Anesth Analg. 2020;130(6):1493–503. https://doi.org/10.1213/ane.0000000000004735.
Gill TM, Baker DI, Gottschalk M, Gahbauer EA, Charpentier PA, de Regt PT, Wallace SJ. A prehabilitation program for physically frail community-living older persons. Arch Phys Med Rehabil. 2003;84(3):394–404. https://doi.org/10.1053/apmr.2003.50020.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–62. https://doi.org/10.1016/s0140-6736(12)62167-9.
Picca A, Coelho-Junior HJ, Calvani R, Marzetti E, Vetrano DL. Biomarkers shared by frailty and sarcopenia in older adults: a systematic review and meta-analysis. Ageing Res Rev. 2022;73:101530. https://doi.org/10.1016/j.arr.2021.101530.
da Silva VD, Tribess S, Meneguci J, Sasaki JE, Garcia-Meneguci CA, Carneiro JAO, Virtuoso JS. Jr. Association between frailty and the combination of physical activity level and sedentary behavior in older adults. BMC Public Health. 2019;19(1):709. https://doi.org/10.1186/s12889-019-7062-0.
Apóstolo J, Cooke R, Bobrowicz-Campos E, Santana S, Marcucci M, Cano A, Vollenbroek-Hutten M, Germini F, D’Avanzo B, Gwyther H, et al. Effectiveness of interventions to prevent pre-frailty and frailty progression in older adults: a systematic review. JBI Database System Rev Implement Rep. 2018;16(1):140–232. https://doi.org/10.11124/jbisrir-2017-003382.
Yoshida G, Boissiere L, Larrieu D, Bourghli A, Vital JM, Gille O, Pointillart V, Challier V, Mariey R, Pellisé F, et al. Advantages and disadvantages of adult spinal deformity Surgery and its impact on Health-Related Quality of Life. Spine (Phila Pa 1976). 2017;42(6):411–9. https://doi.org/10.1097/brs.0000000000001770.
Blondel B, Schwab F, Ungar B, Smith J, Bridwell K, Glassman S, Shaffrey C, Farcy JP, Lafage V. Impact of magnitude and percentage of global sagittal plane correction on health-related quality of life at 2-years follow-up. Neurosurgery. 2012;71(2):341–8. https://doi.org/10.1227/NEU.0b013e31825d20c0. discussion 348.
Smith MA. The Role of Shared decision making in patient-centered care and Orthopaedics. Orthop Nurs. 2016;35(3):144–9. https://doi.org/10.1097/nor.0000000000000243.
Charles C, Whelan T, Gafni A. What do we mean by partnership in making decisions about treatment? BMJ. 1999;319(7212):780–2. https://doi.org/10.1136/bmj.319.7212.780.
Moskven E, Charest-Morin R, Flexman AM, Street JT. The measurements of frailty and their possible application to spinal conditions: a systematic review. Spine J. 2022. https://doi.org/10.1016/j.spinee.2022.03.014.
Acknowledgements
We are grateful to Euna Ju of the research staff for supporting this study.
Funding
This work was supported by the National Research Foundation of Korea grant to WB, which is funded by the Korea government [Ministry of Science and ICT; grant number NRF-2021R1G1A1093450].
Author information
Authors and Affiliations
Contributions
Conceptualization, Methodology, Formal analysis, Investigation: WB, YK; Software, Visualization: WB; Writing—Original draft: WB, YK; Writing—reviewing & Editing: WB, YK, SP; Supervision: YK; Funding acquisition: WB.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Baek, W., Park, SY. & Kim, Y. Impact of frailty on the outcomes of patients undergoing degenerative spine surgery: a systematic review and meta-analysis. BMC Geriatr 23, 771 (2023). https://doi.org/10.1186/s12877-023-04448-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04448-2